Pharmacogenomics: How Your Genes Affect Your Medications
When you take a pill, your body doesn't treat it the same way everyone else does. That’s because of pharmacogenomics, the study of how your genes influence how your body processes medications. Also known as personalized medicine, it’s why one person can take a standard dose of a drug and feel fine, while another gets sick from the same amount. This isn’t about allergies or mistakes—it’s biology written in your DNA.
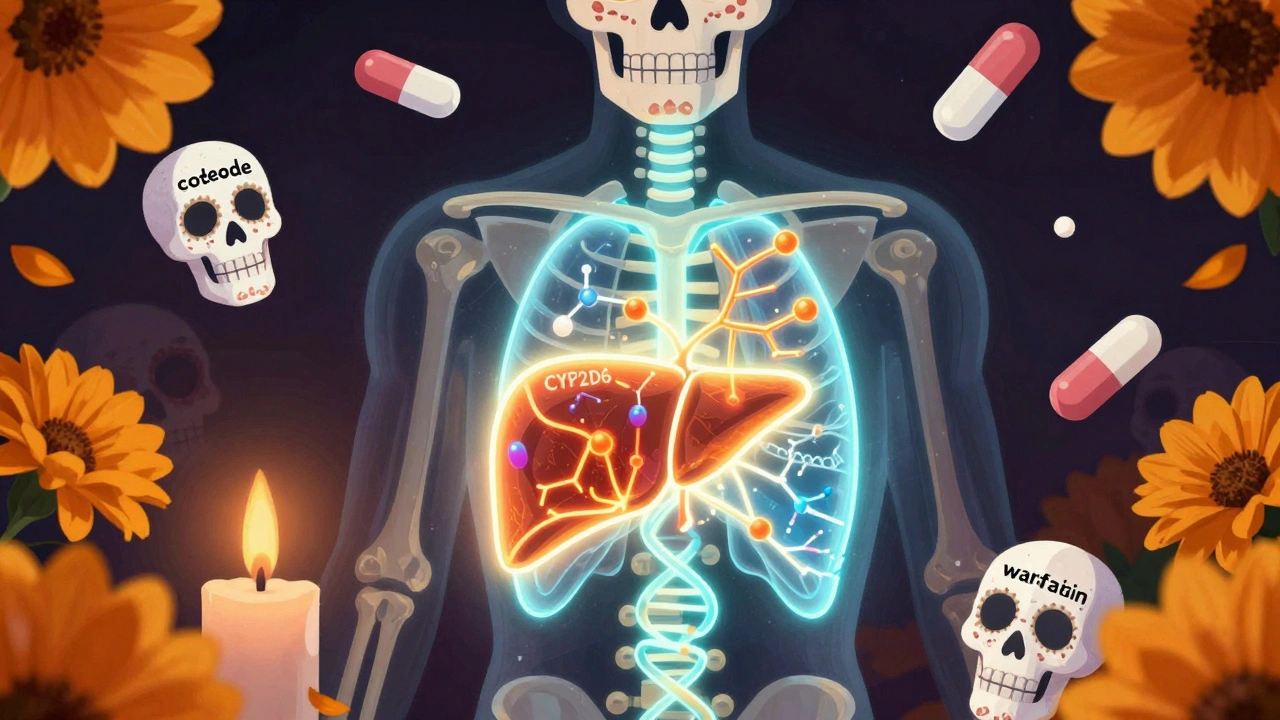
At the heart of this are enzymes like the CYP450 enzymes, a family of liver proteins that break down most drugs. Some people have gene variants that make these enzymes work too fast, so the drug leaves their system before it can help. Others have slow versions, causing drugs to build up to toxic levels. That’s why genetic testing for drugs, a simple cheek swab or blood test that checks for these variations, is becoming part of routine care for medications like blood thinners, antidepressants, and painkillers. For example, if you’re prescribed clopidogrel (Plavix), your doctor might check your genes first—because if you’re a slow metabolizer, the drug won’t work at all.
This isn’t just theoretical. The same gene that affects how you process clopidogrel also changes how you respond to codeine, statins, and even some cancer drugs. A person with a certain variant might need double the dose of a medication to get relief, while someone else could overdose on a standard dose. That’s why doctors now look at your genetic profile when choosing between similar drugs—like picking between two antidepressants based on your metabolism, not just symptoms. And it’s not just about avoiding side effects. It’s about saving time, money, and lives by getting the right drug right the first time.
You’ll find real-world examples of this in the posts below. One article explains how colchicine can turn deadly when mixed with certain antibiotics because of CYP450 interference. Another shows why milk thistle, a popular liver supplement, can mess with how your body handles prescription drugs. There’s even a piece on how fentanyl patches behave differently in people with certain genetic traits that affect drug absorption. These aren’t random cases—they’re all connected by pharmacogenomics. Whether you’re managing chronic pain, taking heart meds, or just trying to avoid a bad reaction, understanding how your genes shape your response to drugs isn’t science fiction. It’s the new standard of care.