Drug Metabolism Genes: How Your DNA Affects Medication Response
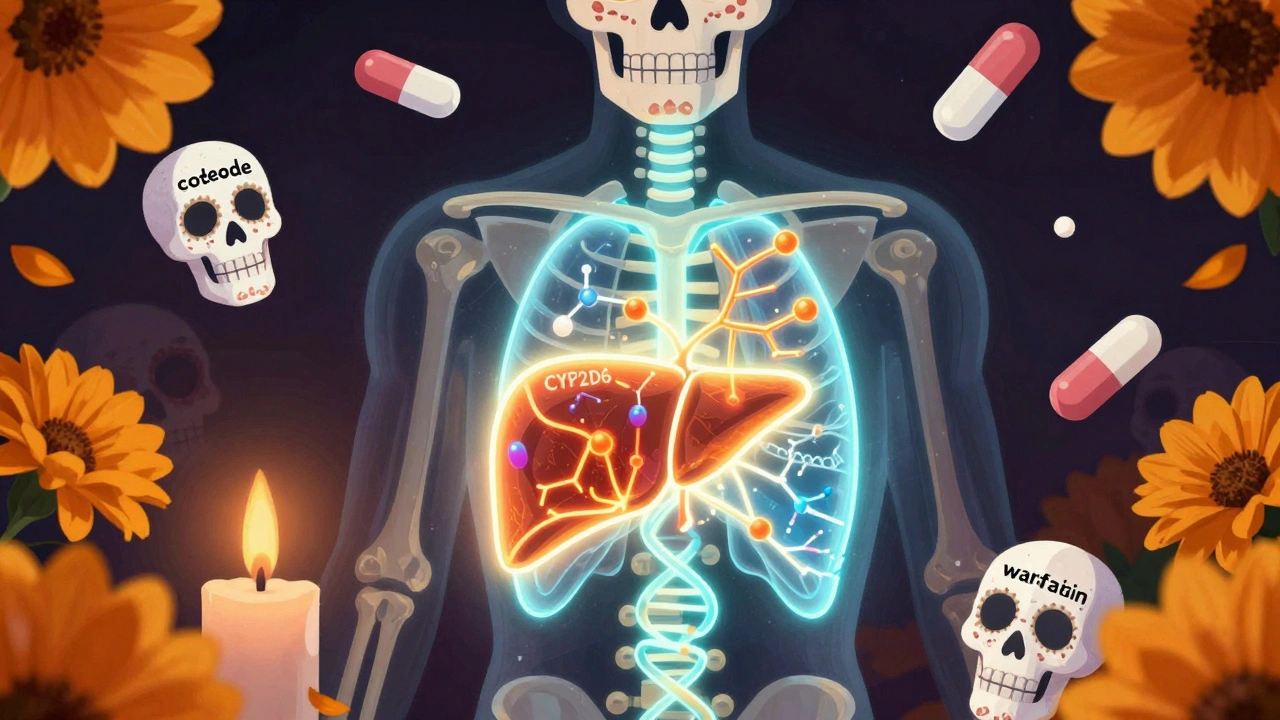
When you take a pill, your body doesn’t just absorb it—it drug metabolism genes, genetic variants that control how your liver breaks down medications. Also known as pharmacogenetics, this field explains why two people taking the same dose of the same drug can have wildly different outcomes—one gets relief, the other gets sick. These genes, especially those in the CYP450 enzyme family, a group of liver proteins that process over 70% of all prescription drugs, act like molecular gatekeepers. If your version of CYP3A4 or CYP2D6 is slow, the drug builds up and causes side effects. If it’s fast, the drug vanishes before it can work.
That’s why some people crash after a normal dose of codeine, while others feel nothing. Codeine needs to be turned into morphine by CYP2D6—and if you’re a poor metabolizer, it won’t work. If you’re an ultra-rapid metabolizer, you could turn a single pill into a dangerous overdose. Same with clopidogrel, a blood thinner: if your CYP2C19 gene is broken, the drug won’t prevent clots, and you’re at risk for a heart attack. This isn’t rare. About 90% of people have at least one gene variant that changes how they respond to meds. Even common supplements like milk thistle or fish oil can interfere with these enzymes, making your prescription less effective—or more toxic. And it’s not just about liver enzymes. Genes that control how drugs move in and out of cells, like P-glycoprotein, a transporter that pushes drugs out of cells and affects absorption and brain penetration, also play a huge role. That’s why colchicine becomes deadly with certain antibiotics—it’s not the antibiotic’s fault. It’s your genes letting the drug pile up.
What you’ll find below isn’t theory. These are real cases: someone overdosing from a fentanyl patch because their body couldn’t clear it fast enough, someone with liver disease reacting badly to a common painkiller, another person whose blood pressure meds failed because their genes made them useless. These aren’t outliers. They’re predictable—if you know what to look for. The posts here show how genetic differences shape everything from migraine relief to heart meds to diabetes control. You’ll learn which drugs are most affected, how to spot the warning signs, and what to ask your doctor before you take your next prescription. This isn’t about guessing. It’s about understanding the code inside you.