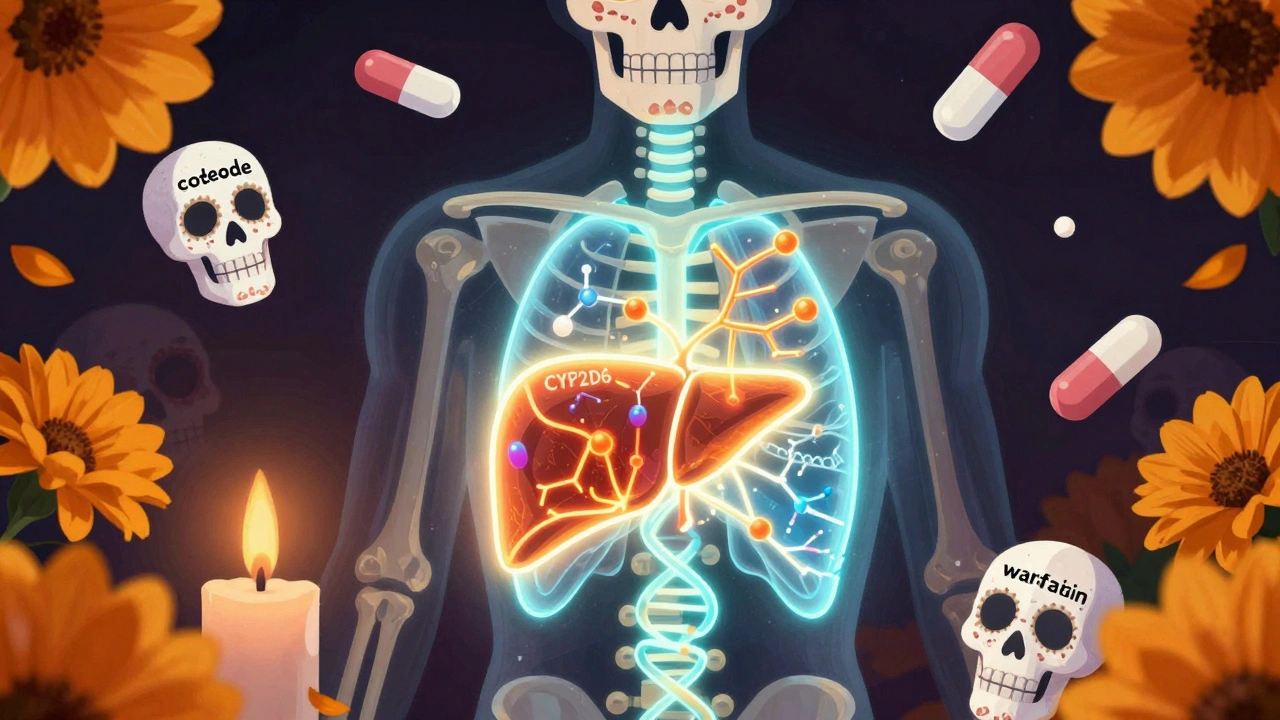
CYP2D6: How This Liver Enzyme Affects Your Medications
When you take a pill, your body doesn’t just absorb it and call it a day. It breaks it down—mostly in the liver—and one of the most important players in that process is CYP2D6, a liver enzyme that metabolizes about 25% of all prescription drugs. Also known as cytochrome P450 2D6, it’s the reason why two people taking the same dose of the same drug can have completely different experiences. Some people break down meds fast, others slow—and it’s not about how much they weigh or how healthy they are. It’s genetics.
CYP2D6 doesn’t work alone. It’s part of a family of enzymes that handle everything from painkillers to antidepressants to heart meds. If you’re on CYP2D6-dependent drugs like codeine, tramadol, fluoxetine, or metoprolol, your version of this enzyme decides whether the drug works, causes side effects, or does nothing at all. People with poor metabolism (called poor metabolizers) can build up toxic levels even at normal doses. Ultra-rapid metabolizers might clear the drug so fast it never works. That’s why some folks get dizzy on a low dose of a beta-blocker while others need triple the amount just to feel anything.
This isn’t just theory. Studies show up to 1 in 10 people of European descent are poor metabolizers of CYP2D6. In some Asian populations, ultra-rapid metabolism is even more common. And it’s not just about the drug itself—some meds can block or boost CYP2D6. Take a common antibiotic like quinidine or an antifungal like fluconazole, and suddenly your painkiller stops working or becomes dangerous. That’s why drug interactions aren’t just about stomach upset—they’re about your body’s ability to process what you’re taking.
Things get even more layered when you mix this with other enzymes like CYP3A4, which shows up in posts about colchicine and macrolides, or milk thistle interfering with liver metabolism. These aren’t random connections. They’re part of the same system. Your liver is a factory, and CYP2D6 is one of the main assembly lines. If it’s broken, clogged, or running too fast, everything downstream gets messed up.
You won’t find CYP2D6 on your pharmacy label. But if you’ve ever wondered why a drug worked for your friend but not you, or why your doctor changed your dose after a blood test, this enzyme is probably why. The posts below dive into real cases—like how fentanyl patches react to heat, why certain antibiotics turn colchicine deadly, and how milk thistle can mess with your meds. They all tie back to this one invisible player in your liver. You don’t need to be a scientist to understand it. You just need to know it exists—and that your body’s way of handling drugs might be very different from everyone else’s.