Prevent Heartburn During Pregnancy: Effective Tips for Expecting Moms
Learn practical, doctor‑approved tips to stop heartburn during pregnancy. From diet tweaks and safe antacids to when to see a doctor, this guide keeps moms‑to‑be comfortable.
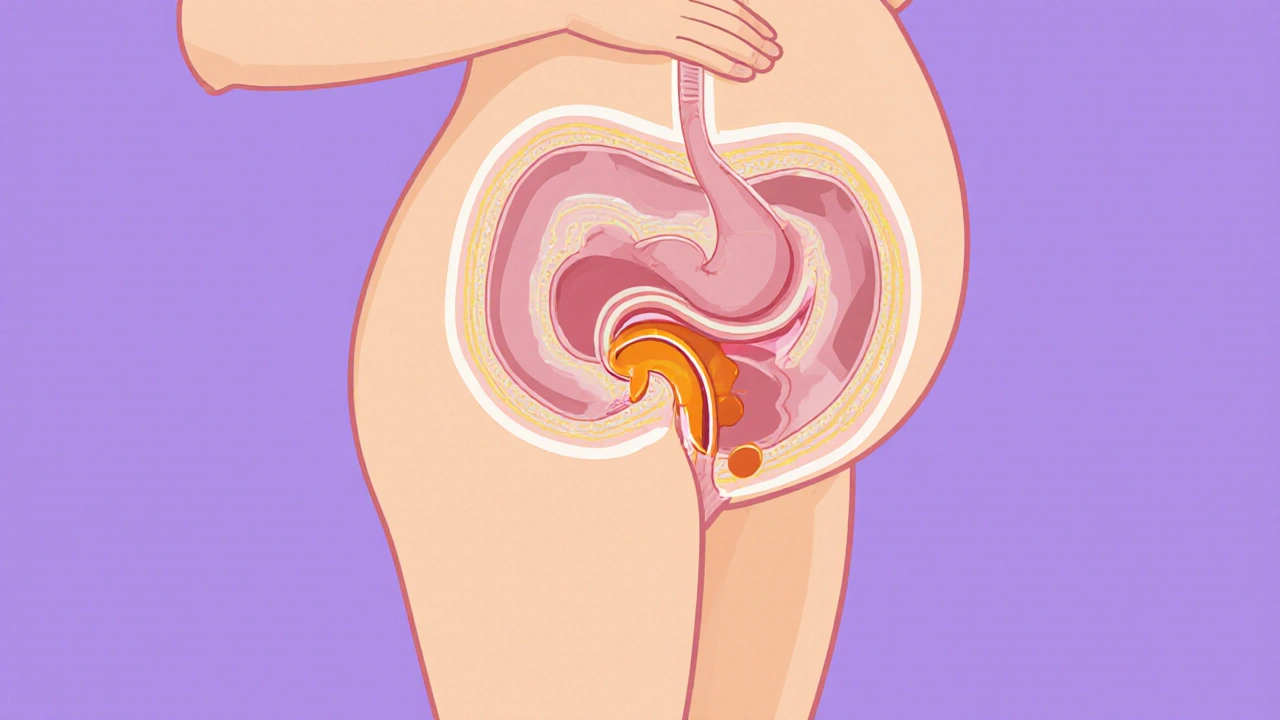
When dealing with acid reflux pregnancy, the rise of stomach acid into the esophagus that many expectant moms experience. Also called pregnancy heartburn, this condition often shows up as heartburn, a burning sensation behind the breastbone. Over‑the‑counter antacids work by neutralizing stomach acid, while prescription proton pump inhibitors (PPIs) reduce acid production at the source. Understanding how these pieces fit together helps you choose safe relief without compromising your baby.
Hormones like estrogen and progesterone rise sharply during pregnancy. acid reflux pregnancy becomes more likely because progesterone relaxes the lower esophageal sphincter (LES), the muscle that normally keeps acid down. When the LES loosens, stomach contents can splash back up, especially after meals. This hormone‑induced relaxation explains why many women notice heartburn for the first time in their second trimester, even if they never had it before. The growing uterus also adds pressure on the stomach, pushing acid toward the esophagus. Together, hormone‑mediated LES relaxation and mechanical pressure create the perfect storm for reflux.
Knowing the root causes lets you target the right solutions. If the LES is the weak spot, lifestyle tweaks that reduce pressure can make a huge difference. If hormones are the main driver, safe medications become a valuable backup. Both approaches work best when you talk with your OB‑GYN, who can guide you on what's appropriate at each stage of pregnancy.
One of the easiest changes is to watch what you eat and when. Large, fatty meals sit in the stomach longer, giving acid more time to leak. Choosing smaller, more frequent meals keeps the stomach from over‑filling. Staying upright for at least an hour after eating helps gravity keep acid where it belongs. Elevating the head of the bed by 6‑10 inches can also curb nighttime symptoms, as the angle reduces the chance of reflux while you lie down.
Food choices matter, too. While spicy dishes, citrus, and chocolate are often blamed, the real culprits are high‑fat foods and carbonated drinks that relax the LES further. Swapping fried snacks for a handful of almonds, sipping water instead of soda, and adding ginger to meals can ease discomfort. Simple swaps like these fit easily into a prenatal diet plan and don’t require any extra prep time.
When diet and positioning aren’t enough, antacids become a go‑to option. Calcium‑carbonate antacids (like Tums) are generally safe and even add a bit of calcium for your baby’s bones. However, it’s best to avoid excessive aluminum‑ or magnesium‑based formulas, which can cause constipation or diarrhea. A typical safe dose is 2‑4 tablets after meals, but always double‑check with your health provider before starting any new pill.
If symptoms persist, doctors may prescribe H2 blockers (such as ranitidine) or PPIs (like omeprazole). These drugs belong to FDA pregnancy categories that suggest they’re low risk when used short‑term. PPIs are especially effective because they lower overall acid production, giving the LES a break. Still, the rule of thumb is to use the lowest effective dose for the shortest time needed. Your OB‑GYN can help you weigh the benefits against any potential risks.
Integrating reflux management into prenatal care means regular check‑ins. Bring up any new or worsening heartburn at each appointment. Your provider can monitor your weight gain, blood pressure, and vitamin levels to ensure the antacid or PPI won’t interfere with other aspects of your pregnancy. In some cases, a referral to a gastroenterologist might be warranted, especially if you have a history of severe GERD before pregnancy.
There are plenty of myths floating around, too. Many expectant moms think that coffee or chocolate will always trigger heartburn, yet studies show that individual tolerance varies widely. The same goes for caffeine; a small cup may be fine, while a large espresso could be the tipping point. Listening to your own body and keeping a symptom diary can help you pinpoint true triggers versus old beliefs.
Below you’ll find a curated collection of articles that dive deeper into each of these topics. From detailed comparisons of antacids and PPIs to lifestyle hacks that fit a busy pregnancy schedule, the posts are designed to give you actionable insights you can start using today.
Learn practical, doctor‑approved tips to stop heartburn during pregnancy. From diet tweaks and safe antacids to when to see a doctor, this guide keeps moms‑to‑be comfortable.