Pregnancy Heartburn Trigger Calculator
Find Your Personal Triggers
Answer these questions to identify which factors most likely contribute to your heartburn. Based on your responses, we'll provide personalized management tips.
Key Triggers Identified
If you're battling heartburn during pregnancy, these tips can help you stay comfortable and enjoy your bump without the burning after‑taste.
What Causes Heartburn in Pregnancy?
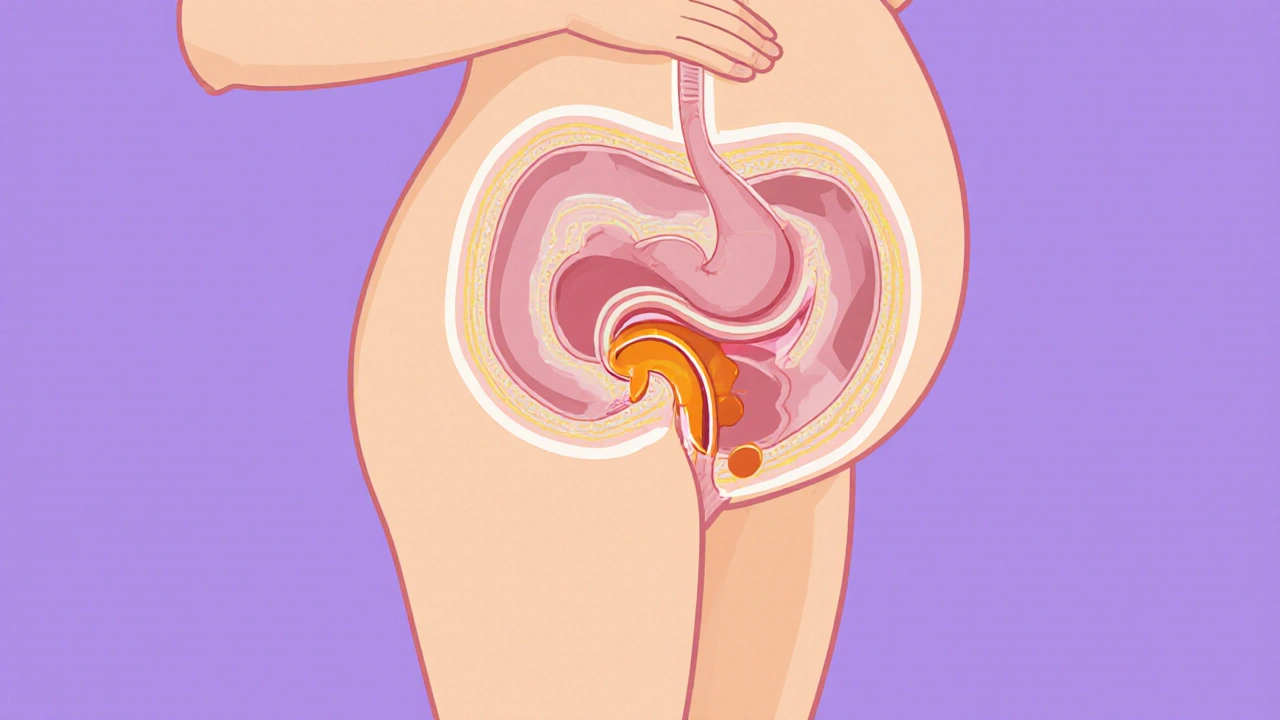
During pregnancy, the hormone Progesterone relaxes the lower esophageal sphincter, allowing stomach acid to flow back into the esophagus. At the same time, the growing uterus pushes the stomach upward, increasing pressure on the digestive tract. This perfect storm turns a normal acid reflux into frequent, uncomfortable heartburn a burning sensation behind the breastbone caused by stomach acid irritating the esophagus for many moms‑to‑be.
Identify Common Dietary Triggers
Not every food bothers everyone, but research shows a handful of culprits that consistently provoke reflux in pregnant women:
- Spicy foods (chili, pepper, curry)
- Citrus fruits and juices (orange, grapefruit)
- Tomato‑based sauces and ketchup
- Chocolate and peppermint
- Fried or fatty meals
- Caffeinated drinks (coffee, tea, soda)
Keeping a simple food diary for a week helps you pinpoint which of these dietary triggers specific foods or beverages that increase stomach acidity and relax the esophageal valve affect you most.
Lifestyle Tweaks That Really Work
Small habit changes can slash heartburn episodes without any medication:
- Eat smaller, more frequent meals - aim for 5-6 light portions rather than three big plates.
- Finish eating at least two hours before lying down; if you need a snack later, choose a low‑fat option like a banana.
- Elevate the head of your bed by 6-8 inches using a wedge pillow; gravity keeps acid where it belongs.
- Wear loose‑fitting clothing around the waist to avoid extra pressure on the abdomen.
- Stay upright for 30 minutes after meals; a gentle walk does the trick.
These adjustments address the two main physiological drivers-sphincter relaxation and increased intra‑abdominal pressure-making the reflux pathway harder to trigger.

Safe Over‑the‑Counter Options
When lifestyle alone isn’t enough, certain antacids are considered safe for most pregnancies. Always check the label for calcium carbonate, which also supplies needed calcium for fetal bone development.
| Remedy | How It Works | Pregnancy Safety | Typical Use |
|---|---|---|---|
| Calcium carbonate antacid neutralizes stomach acid by supplying calcium | Immediate acid neutralization | Generally safe; provides extra calcium | 1-2 tablets after meals, up to 4×daily |
| H2 blocker (e.g., ranitidine) reduces acid production by blocking histamine receptors | Longer‑lasting reduction of acid | Approved for short‑term use; discuss with OB‑GYN | 10mg once daily before bedtime |
| Proton pump inhibitor (PPI) inhibits the final step of acid secretion | Strong, prolonged acid suppression | Reserved for severe cases; physician oversight required | 5mg once daily, usually for < 8weeks |
| Ginger tea has mild anti‑nausea and digestive soothing properties | Natural soothing effect | Safe in moderate amounts (1-2cups/day) | Warm tea after meals |
Remember, any medication-prescription or OTC-should be approved by your prenatal care provider.
When to Call Your Healthcare Provider
Most heartburn is manageable, but seek professional advice if you notice any of these red flags:
- Persistent vomiting or inability to keep food down \n
- Difficulty swallowing or a feeling of food sticking in the throat
- Weight loss despite a normal pregnancy diet
- Severe chest pain that radiates to the jaw or arm (could signal cardiac issues)
These symptoms may signal a more serious condition like gastroesophageal reflux disease (GERD chronic reflux that can damage the esophagus over time) or a medication side‑effect that needs adjustment.

Quick Checklist for a Heartburn‑Free Day
- Start the day with a glass of water; avoid coffee.
- Choose whole‑grain toast, oatmeal, or Greek yogurt for breakfast.
- Snack on almonds or an apple, not citrus.
- Keep lunch light: grilled chicken, steamed veggies, quinoa.
- After dinner, take a short walk and stay upright for at least 30minutes.
- Use a wedge pillow at night; avoid lying flat.
- Carry calcium carbonate tablets for on‑the‑go relief.
This routine targets the two main contributors to reflux-acid exposure and pressure-so you can focus on the joy of pregnancy rather than the burn.
Frequently Asked Questions
Can I take Tums throughout my entire pregnancy?
Tums (calcium carbonate) are safe for most pregnant women and provide extra calcium, but it’s best to stay under 2,500mg of calcium per day from all sources. Check with your OB‑GYN if you need a higher dose.
Are peppermint teas a good idea?
Peppermint can relax the lower esophageal sphincter, potentially worsening reflux. Opt for ginger or chamomile instead.
What’s the safest prescription option if OTC drugs fail?
A short course of an H2 blocker like ranitidine is often recommended first, followed by a low‑dose PPI if symptoms remain severe. Both require doctor approval.
Should I avoid all fried foods?
Fried and high‑fat foods delay stomach emptying, increasing pressure on the sphincter. Cutting back substantially reduces heartburn frequency.
Is heartburn a sign of a bigger problem for my baby?
Rarely. Heartburn itself doesn’t affect fetal health, but severe, untreated GERD can lead to nutritional deficits for the mother. Keep symptoms in check and follow medical advice.

Iain Clarke
October 16, 2025 AT 09:33It's worth noting that keeping a food diary can pinpoint personal triggers more accurately than generic lists. Small, frequent meals and staying upright after eating are especially beneficial during the second trimester. Also, a wedge pillow is a simple tool that many expectant mothers find effective for reducing night‑time reflux.
Courtney Payton
October 17, 2025 AT 13:20One shoudn't just ignore the scientific consensus on pregnancy‑safe antacids; ignoring it is a mild act of negligence toward your unborn child. The body is a temple, and respecting its signals is a moral duty.
Muthukumaran Ramalingam
October 18, 2025 AT 17:06Honestly, most of the tips in the article are just common sense that I have heard from my aunt who had three kids. Eating smaller meals? That's basic. Elevating the head of the bed sounds like a good idea but many people won't bother buying a wedge pillow. The list of trigger foods is also pretty standard, and if you already know you hate spicy stuff you don't need a table. Overall, the advice works but it's nothing groundbreaking.
Garrett Williams
October 19, 2025 AT 20:53Great quick checklist for busy moms.
Charmaine De Castro
October 21, 2025 AT 00:40Thanks for compiling those practical steps; the suggestion to start the day with water instead of coffee really resonates. I also love the idea of a short walk after dinner-it’s a simple habit that can fit into any schedule.
Mark Mendoza
October 22, 2025 AT 04:26Adding a calcium carbonate antacid can also contribute to daily calcium needs 📈. Just be sure to stay within the recommended dosage and check with your provider before combining with other supplements 😊.
Dan Tourangeau
October 23, 2025 AT 08:13These recommendations are solid and easy to integrate. Remember to monitor portion sizes and stay hydrated.
Bernard Valentinetti
October 24, 2025 AT 12:00Indeed, the physiologic mechanisms-namely, progesterone‑induced sphincter relaxation and increased intra‑abdominal pressure-constitute a synergistic cascade, rendering reflux inevitable unless mitigated; thus, the article's emphasis on lifestyle modulation is not merely anecdotal but scientifically substantiated!!! 🍃
Kenneth Obukwelu
October 25, 2025 AT 15:46Behold! The humble wedge pillow rises like a champion against the fiery dragons of heartburn, lifting not just heads but spirits! With each upright step after supper, we march toward a realm where the burning abyss is tamed, and the pregnancy journey becomes a saga of triumph over the acid tide.
Josephine hellen
October 26, 2025 AT 18:33Pregnancy is a remarkable journey, and dealing with heartburn should never feel like an insurmountable obstacle. I have tried countless remedies, from ginger tea to calcium tablets, and each one taught me something valuable about listening to my body. The first lesson was to recognize that the timing of meals matters profoundly; eating too close to bedtime invites the dreaded night‑time burn. Second, I discovered that the texture of food can influence reflux, with smoother options like oatmeal causing less irritation than chunky, fried dishes. Third, staying hydrated throughout the day helps dilute stomach acid and promotes smoother digestion. Fourth, incorporating a gentle 20‑minute walk after dinner not only aids in gravity‑assisted gastric emptying but also lifts the mood during those hormonal swings. Fifth, I learned to replace caffeine with herbal alternatives, particularly chamomile, which soothes the stomach without the jittery side effects. Sixth, adjusting clothing to looser fits reduced the pressure on my abdomen, allowing the sphincter to function more effectively. Seventh, I experimented with small amounts of almond butter as a low‑fat snack, and it proved satisfying without triggering reflux. Eighth, I kept a simple notebook to track which foods sparked the burn, and over weeks a clear pattern emerged that helped me fine‑tune my diet. Ninth, I consulted my OB‑GYN before starting any over‑the‑counter antacid, ensuring safety for both me and my baby. Tenth, I embraced the wedge pillow as a nightly ally, finding that a slight incline dramatically lessened the nocturnal flare‑ups. Eleventh, I made a habit of sipping warm water with a pinch of baking soda when a sudden wave hit, which provided quick, temporary relief. Twelfth, I learned that stress management through deep breathing exercises can lower the overall acid production. Thirteenth, I discovered that certain probiotic yogurts support gut health, reducing overall acidity. Fourteenth, I stayed vigilant for warning signs such as persistent vomiting, which prompted immediate medical attention. Finally, with patience, consistency, and a bit of trial‑and‑error, I turned heartburn from a daily nuisance into an occasional, manageable occurrence, allowing me to fully enjoy the miracle of pregnancy.
Northern Lass
October 27, 2025 AT 22:20While the prevailing medical consensus endorses calcium carbonate as a benign antacid, one must consider the less discussed ramifications of widespread pharmaceutical endorsement. It is plausible that corporate interests subtly influence the recommendation landscape, steering expectant mothers toward products that serve profit motives rather than optimal health outcomes. Consequently, a skeptical examination of all suggested remedies is warranted before acceptance.
Johanna Sinisalo
October 29, 2025 AT 02:06It is encouraging to see evidence‑based strategies being shared, and I recommend integrating these practices gradually to assess individual tolerance. A balanced approach, combining dietary awareness with gentle physical activity, often yields the most sustainable relief.
Nikita Warner
October 30, 2025 AT 05:53Further investigation into the comparative efficacy of H2 blockers versus proton pump inhibitors during the second trimester could provide valuable guidance for clinicians and patients alike. Such data would enhance shared decision‑making and ensure that therapeutic choices align with both maternal comfort and fetal safety.