Mental Health: Practical guides on meds, symptoms and day-to-day care
Mental health affects how you think, feel and handle daily life. This category collects clear info on common conditions, medicines, side effects and when to seek help. You’ll find practical tips you can use right away — not vague theory.
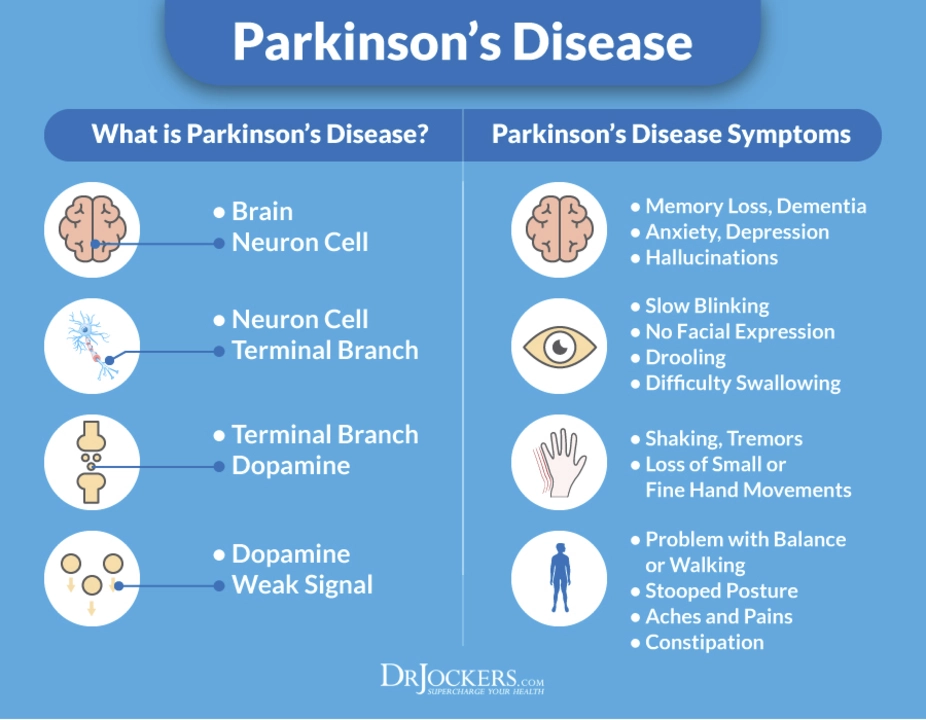
Want a quick example? We cover treatments like loxapine for psychosis in Parkinson’s disease. Early reports and small studies suggest it may ease psychotic symptoms without making motor problems worse, but more research is needed. That’s the kind of focused update you’ll see here: promising, cautious, and linked to clinical context.
Medications and what to watch for
Medications can help a lot, but they come with trade-offs. For antipsychotics and mood stabilizers, pay attention to sedation, blood pressure changes, metabolic effects, and movement symptoms. Some drugs can interact with Parkinson’s medicines or raise heart rhythm risks. Always check drug interactions before starting anything new.
When a new treatment is suggested — say a switch to loxapine — practical steps matter: start low, increase slowly, and monitor both mental symptoms and physical side effects. Keep a symptom diary for two weeks after a change. Note sleep, appetite, tremor, balance and mood swings. That record makes follow-up visits more useful.
How to use this category
Use posts here as a starting point. Each article explains what a medicine does, likely benefits, typical side effects, and real-world warnings. We also link to original studies or case reports when available so you can see the evidence behind a claim.
If an article mentions a promising option for a specific condition — for example, psychosis in Parkinson’s — treat it as something to discuss with your neurologist or psychiatrist, not as a self-prescription. Specialists balance mental benefits with risks to movement and other health issues.
Practical checklist before trying a new psychiatric drug: 1) review current meds for interactions, 2) check cardiac history and ECG if needed, 3) set measurable goals with your doctor, and 4) schedule a follow-up within two weeks.
Emergency signs you should act on fast: sudden worsening of movement, severe dizziness, fainting, fast irregular heartbeat, chest pain, suicidal thoughts, or sudden confusion. Call your healthcare provider or emergency services if these occur.
This category also covers everyday support — how caregivers can help, tips for medication adherence, and ways to talk with doctors so appointments lead to clear action. We keep language simple and advice practical so you can use it now.
Browse posts for condition-specific entries and medication guides. If you want deeper detail, look for articles that cite clinical trials or expert reviews. And whenever you try something new, loop in your prescribing clinician — that keeps care safe and effective.