Most people assume that when a doctor writes a prescription, the pharmacy can swap in a cheaper generic version. That’s usually true - and it saves billions every year. But sometimes, that swap isn’t allowed. When a doctor writes do not substitute on a prescription, it’s not a suggestion. It’s a medical order. And it’s more common than most patients realize.
What Does 'Do Not Substitute' Really Mean?
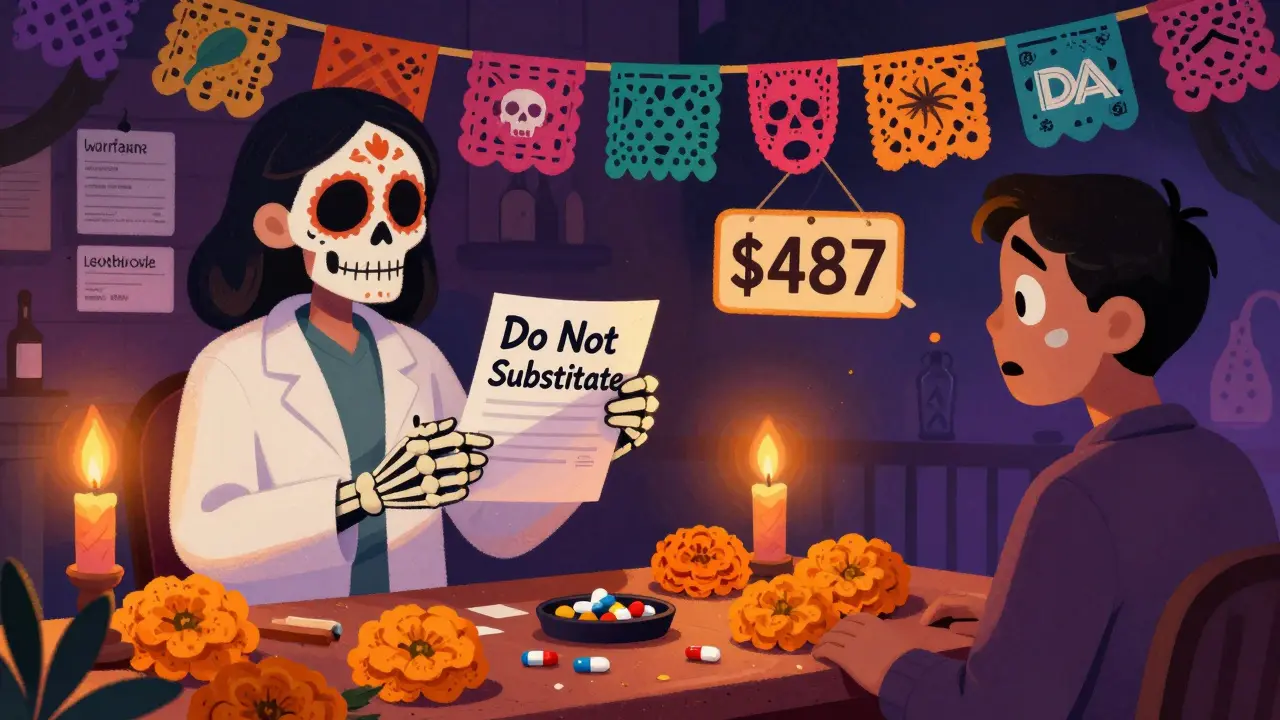
Do not substitute - also called dispense as written or DAW - means the pharmacist must give you the exact brand-name drug the doctor prescribed. No generic version. No alternative. Even if the generic is FDA-approved and costs a fraction of the price. This isn’t about brand loyalty. It’s about safety. The FDA requires generics to match brand drugs in active ingredients, strength, and dosage form. But for some medications, even tiny differences in how the drug is absorbed can cause real problems. These are called narrow therapeutic index drugs. A small change in blood levels can mean the difference between control and crisis. Drugs like warfarin (a blood thinner), levothyroxine (for thyroid conditions), and phenytoin (for seizures) fall into this category. Studies show that switching generics for these drugs can lead to hospitalizations. In 2021, the FDA’s adverse event database recorded over 1,200 cases where generic substitution caused therapeutic failure in patients on NTID medications.Why Can’t All Generics Be Swapped?
The FDA says 99.5% of approved generics are therapeutically equivalent to their brand-name counterparts. That’s true - for most drugs. But equivalence doesn’t always mean interchangeability. For small-molecule drugs (like antibiotics or blood pressure pills), generics are almost always safe to swap. But for biological drugs - things like insulin, rheumatoid arthritis treatments, or cancer therapies - the story is different. These are complex molecules made from living cells. Even minor changes in manufacturing can alter how they work in the body. The FDA has a special label for biosimilars: interchangeable. Only 12 of these have earned that status as of late 2023. That means, out of hundreds of biologic drugs on the market, only a handful can legally be swapped without a doctor’s approval. So when a doctor writes do not substitute on a biologic prescription, it’s often because no interchangeable version exists. And it’s not just about the active ingredient. Some drugs come in special delivery systems - inhalers, prefilled pens, patches. Even if the chemical is the same, changing the delivery device can change how the drug is absorbed. Forty-three states ban substitution in these cases, even if the generic has the same active ingredient.How Do Doctors Legally Say 'Do Not Substitute'?
It’s not enough to just say it out loud. The law requires clear, written instructions on the prescription. Each state has its own rules, but most require one of these phrases:- Do not substitute
- Dispense as written
- DAW
- Medically necessary
Why Do Some Doctors Overuse 'Do Not Substitute'?
Here’s the uncomfortable truth: not every do not substitute order is medically necessary. The American Medical Association found that 8-12% of all prescriptions in 2022 had DNS labels. But experts like Dr. Aaron Kesselheim from Harvard say that in some drug classes, DNS rates are hitting 25-30%. That’s far above what clinical evidence supports. Why? Sometimes it’s habit. Sometimes it’s lack of awareness. And sometimes, it’s pressure from drug companies. Brand-name manufacturers have a financial incentive to keep patients on their expensive products. They may provide materials or training that overstate the risks of generics - even for drugs where the evidence shows no real difference. The American College of Physicians warned in 2022 that inappropriate DNS use adds $15.7 billion in avoidable costs to the U.S. healthcare system every year. That’s money that could go to other patients, other treatments, other needs.What Happens When You Get a 'Do Not Substitute' Prescription?
You’ll notice it right away at the pharmacy. Instead of paying $10 for a generic, you’re looking at $487 for the brand. That’s not a typo. A 2022 study in Health Affairs found that DNS prescriptions cost 237% more on average than generics. Many patients don’t understand why. A Kaiser Family Foundation survey in 2022 found that 68% of people receiving DNS prescriptions didn’t know the cost difference until they got to the counter. Forty-two percent said they would’ve chosen the generic if they’d been told. If you get a DNS prescription and the price shocks you, ask questions:- Why can’t I use the generic?
- Is this because of a previous reaction?
- Is there a biosimilar or alternative?
- Can we check if my insurance has a prior authorization process?
Insurance and the 'Do Not Substitute' Problem
Insurance companies hate DNS prescriptions. They’re expensive. And they’re often not pre-approved. In 2022, 73% of community pharmacists reported that insurance systems rejected DNS claims 15-20% of the time. Why? Because the system doesn’t recognize the code, or the pharmacy didn’t enter the right DAW number (there are 10 different codes for substitution status). This creates delays. You wait hours - sometimes days - for the pharmacy to call the doctor, get a new prescription, or file an appeal. In the meantime, you go without your medicine. Medicare Part D has the highest DNS rates - 12.7% - compared to 8.3% for commercial insurance. That’s partly because Medicare covers more older adults, who are more likely to be on NTID drugs like warfarin or levothyroxine.
What’s Changing?
The tide is turning. In 2023, 18 states introduced bills to limit DNS use to only clinically justified cases. Seven states now require prior authorization before insurers will pay for a brand drug when a generic is available. The FDA is investing $50 million over the next five years to study bioequivalence in narrow therapeutic index drugs. If they find that some generics are safer than previously thought, DNS rates for those drugs could drop by 25%. The 2022 Inflation Reduction Act also requires Medicare to track DNS usage starting in 2024. That means doctors and pharmacies will be held more accountable. Overuse won’t be invisible anymore.What Should You Do?
If your doctor writes do not substitute on your prescription:- Ask why. Don’t assume it’s automatic.
- Check if you’ve had a bad reaction to a generic before.
- Look up the drug in the FDA’s Orange Book - it lists which generics are approved as equivalent.
- Ask your pharmacist if there’s an interchangeable biosimilar available.
- If the cost is too high, ask your doctor if they can help with a patient assistance program.
Final Thought
Do not substitute isn’t a loophole. It’s a safety tool. Used correctly, it saves lives. Used carelessly, it wastes money and confuses patients. The goal isn’t to eliminate brand drugs. It’s to make sure they’re used only when they’re truly needed. The system works best when doctors, pharmacists, and patients all understand the why behind the prescription. Not just the what.Can a pharmacist refuse to fill a 'do not substitute' prescription?
No, a pharmacist cannot refuse to fill a valid 'do not substitute' prescription. If the prescription is properly written with the required language and signature, the pharmacist is legally required to dispense the brand-name drug as written. Refusing could result in disciplinary action from the state pharmacy board.
Is 'do not substitute' the same as 'brand necessary'?
Yes, they mean the same thing. 'Brand necessary' is just another term used in some states or electronic systems to indicate that the prescriber wants the brand-name drug dispensed. Both phrases legally prevent generic substitution.
Why are biologics treated differently than regular generics?
Biologics are made from living cells, not chemicals. Their structure is far more complex, and even tiny changes in manufacturing can affect how they work in the body. Unlike small-molecule generics, which must match the brand within 80-125% of absorption, biosimilars must prove they are 'interchangeable' - meaning they can be swapped without any risk of reduced safety or effectiveness. Only 12 have achieved this status as of 2023.
Can I switch from a brand to a generic if my doctor wrote 'do not substitute'?
No, not without a new prescription. Once a 'do not substitute' order is written and signed, it’s legally binding. If you want to switch to a generic, you need to ask your doctor to write a new prescription without the DNS notation. Never switch on your own - especially with narrow therapeutic index drugs.
Does 'do not substitute' mean the drug is better?
Not necessarily. It means the prescriber believes the brand version is safer or more effective for your specific case - often because of past reactions, the drug’s narrow therapeutic index, or delivery system differences. For most drugs, generics are just as safe and effective. The label is about clinical need, not quality.
Are there any drugs where 'do not substitute' is always required?
Yes. For drugs with a narrow therapeutic index - like levothyroxine, warfarin, phenytoin, cyclosporine, and digoxin - many doctors and pharmacists default to 'do not substitute' because small changes in blood levels can cause serious side effects. Even though generics are approved, the risk of instability is higher, so many providers prefer to keep patients on the same formulation.

Shane McGriff
January 20, 2026 AT 01:12This is one of those topics that gets buried under insurance bureaucracy and pharma lobbying. I’ve been on levothyroxine for 12 years, and switching generics once gave me palpitations and brain fog for weeks. My endo told me to stick with the brand-and I did. It’s not about cost. It’s about stability. If your body’s been balanced on a knife’s edge, you don’t mess with the blade.
Pharmacists aren’t the enemy here. The system is. They’re stuck between a rock and a hard place: follow the law or risk your license. Meanwhile, patients are left confused, angry, and out of pocket.
Doctors need better training on when DNS is actually needed. Not every patient needs the brand. But for some? It’s the difference between life and a hospital stay. We need clarity-not more red tape.
clifford hoang
January 21, 2026 AT 19:13ALERT: BIG PHARMA IS USING ‘DO NOT SUBSTITUTE’ AS A COVERT TAX ON THE POOR 😱
Think about it. The FDA says generics are ‘equivalent’-but who funds the studies? The same companies that make the brand drugs. They pay for ‘research’ that ‘proves’ generics are risky… for drugs they own.
And now they’ve got doctors scared to switch? Classic. They’ve got the AMA in their back pocket, the FDA on payroll, and pharmacies too scared to question it. Meanwhile, grandma’s insulin costs $487 because ‘science’ says so.
Next they’ll say your water filter ‘must be brand X’ because ‘impurities vary’. 🤡
Wake up, people. This isn’t medicine. It’s capitalism with a stethoscope.
Andy Thompson
January 22, 2026 AT 20:11USA FIRST. If you can’t afford your meds, move to India. They got generics for $2. Here? We pay for quality. Brand drugs are made in the US under strict FDA rules. Generics? Some come from factories in China where they use the same machines that make phone chargers. 🇺🇸💪
Don’t be a sheep. If your doc says ‘do not substitute’, trust them. They didn’t go to med school to help you save $10 on your blood thinner. They went to save your life.
Also, if you’re mad about the price, vote for someone who’ll fix the system-not just whine on Reddit. 🤬
pragya mishra
January 24, 2026 AT 02:21Why do you think your doctor wrote 'do not substitute'? Because you're lucky they even noticed you exist. I had a friend who got switched to a generic for her seizure meds and had a seizure at work. She lost her job. Her husband left. Her kid went to live with her mom. All because someone thought ‘it’s the same chemical’. No. It’s not. Your body remembers. Your brain remembers. Your nerves remember.
Stop treating medicine like a grocery list. You don’t swap out eggs for tofu and call it breakfast. Stop pretending pills are interchangeable.
And if you can’t afford it? Apply for help. Don’t blame the system. Blame yourself for not planning ahead.
kumar kc
January 24, 2026 AT 11:16People who demand generics for warfarin are playing Russian roulette with their lives. Simple as that.
Emily Leigh
January 26, 2026 AT 07:04Okay but… what if the brand drug is just… overpriced because the company owns the patent? And what if the ‘narrow therapeutic index’ is just a convenient excuse to keep people hooked on $500 pills? I mean, if generics are FDA-approved, why are we still treating them like radioactive waste?
Also, why does every single comment here sound like a pharma ad? Who paid you guys? 😏
And don’t even get me started on the ‘emotional attachment’ to a pill brand. I’m not emotionally attached to my Advil. I’m attached to not going broke.
Thomas Varner
January 28, 2026 AT 05:32Just… wow.
So let me get this straight: a drug can be chemically identical, FDA-approved, and still not be ‘interchangeable’ because… the body might react differently? And this is a problem only for certain drugs? And doctors have to manually override their EHRs every single time? And it takes 2.3 minutes per script?
That’s… a lot of tiny, preventable friction.
And then there’s the insurance part. Where the pharmacy has to use the right DAW code, and if they mess it up, the claim gets rejected, and the patient goes without meds for days? That’s not healthcare. That’s a bureaucratic obstacle course with pills at the finish line.
I get that some drugs need the brand. But why is the system so… broken? Why can’t we have a better flag? A smarter algorithm? A simple ‘this one’s fragile’ sticker?
Also, 12 interchangeable biosimilars out of hundreds? That’s… not progress. That’s a system that’s afraid to evolve.
Jacob Cathro
January 30, 2026 AT 01:30so like… if i switch my levothyroxine generic and my heart starts acting up, is that on me? or on the pharmacist? or the doc who didn’t write ‘do not substitute’ properly? or the EHR that auto-selected the generic? or the FDA who approved the generic in the first place? 🤯
also why does every single doc i’ve ever seen just check ‘DAW’ like it’s a checkbox on a form? like… did they even read the patient’s history? or are they just trying to avoid liability? because if i die from a generic, it’s not their fault right? they checked the box.
and also… why is this even a thing? why not just make ALL generics perfect? why do we have this ‘narrow therapeutic index’ crap? is it because the pharma companies didn’t invest enough in R&D? or because the FDA is too lazy to standardize? or is it just… capitalism?
Renee Stringer
January 31, 2026 AT 10:51I’ve seen too many patients get scared off by the price tag and stop taking their meds altogether. That’s the real tragedy here. Not the $487 pill. The person who doesn’t take it because they think they can’t afford it.
Doctors need to have this conversation before the prescription is written. Not after the patient is standing at the counter with a credit card in one hand and a panic attack in the other.
And pharmacies? You know the cost difference. You see the confusion. Don’t just hand over the pill and walk away. Say something. Even just: ‘This is expensive. Let me help you find assistance.’
It’s not about the drug. It’s about the human behind it.
Paul Barnes
February 1, 2026 AT 02:16There is a clear distinction between therapeutic equivalence and interchangeability. The FDA's definition of bioequivalence (80–125% AUC and Cmax) is statistically valid for population-level outcomes but inadequate for individual patients on narrow therapeutic index drugs. Studies demonstrating population equivalence do not guarantee clinical stability in sensitive individuals. The 1,200 adverse events cited are underreported; real-world data suggest a higher incidence. Furthermore, state laws regulating substitution vary widely and are inconsistently enforced, creating a patchwork of legal risk for pharmacists. The burden of manual override in EHR systems is not a technical flaw but a symptom of systemic underinvestment in clinical decision support infrastructure. The $15.7 billion annual cost estimate is plausible but does not account for downstream costs of hospitalization, lost productivity, or caregiver burden. The solution is not to eliminate DAW orders but to standardize them with evidence-based clinical guidelines and integrate them into interoperable clinical decision support systems.