Topical Meloxicam Dosage Estimator
Calculate Your Topical Meloxicam Application
Estimate the appropriate amount of topical meloxicam for your specific pain area and severity level
Recommended Amount
Important Note: This calculator estimates typical application amounts. Always follow your physician's specific dosing instructions and never exceed the recommended amount. Topical meloxicam should not be applied to broken skin or open wounds.
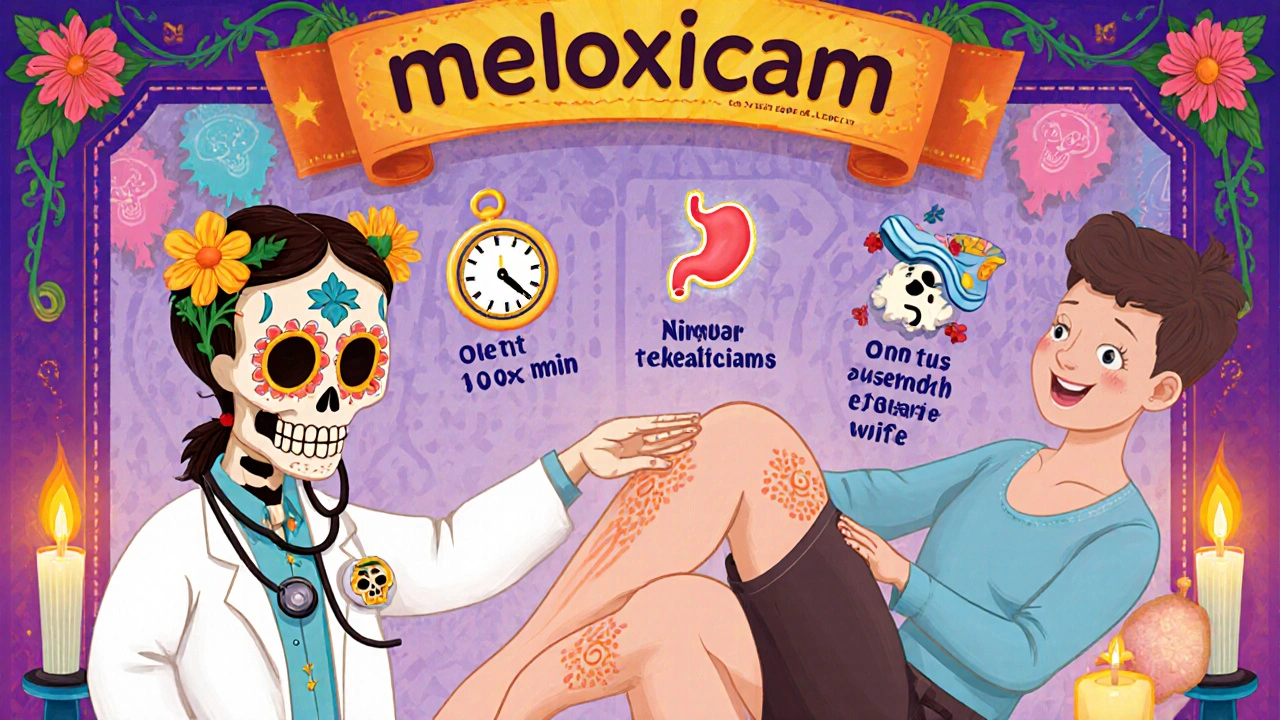
When you think about pain‑killing pills, the first thing that comes to mind is usually a tablet you swallow. What if you could slip the medicine onto the skin right where it hurts? Meloxicam is a prescription‑strength NSAID that’s been used for years in oral form. Now a topical meloxicam cream is emerging, promising the same anti‑inflammatory power without the stomach‑upset that oral NSAIDs can cause. This guide walks you through how the skin‑based version works, who can benefit, and what to watch out for.
What is Meloxicam?
Meloxicam is a non‑steroidal anti‑inflammatory drug (NSAID) that selectively inhibits the enzyme COX‑2, reducing prostaglandin production and therefore inflammation and pain. Originally approved in 2000 for oral tablets and injectables, it’s been a go‑to for osteoarthritis, rheumatoid arthritis, and acute musculoskeletal injuries. Typical oral doses range from 7.5 mg to 15 mg daily, and the drug’s half‑life of about 20 hours allows once‑daily dosing.
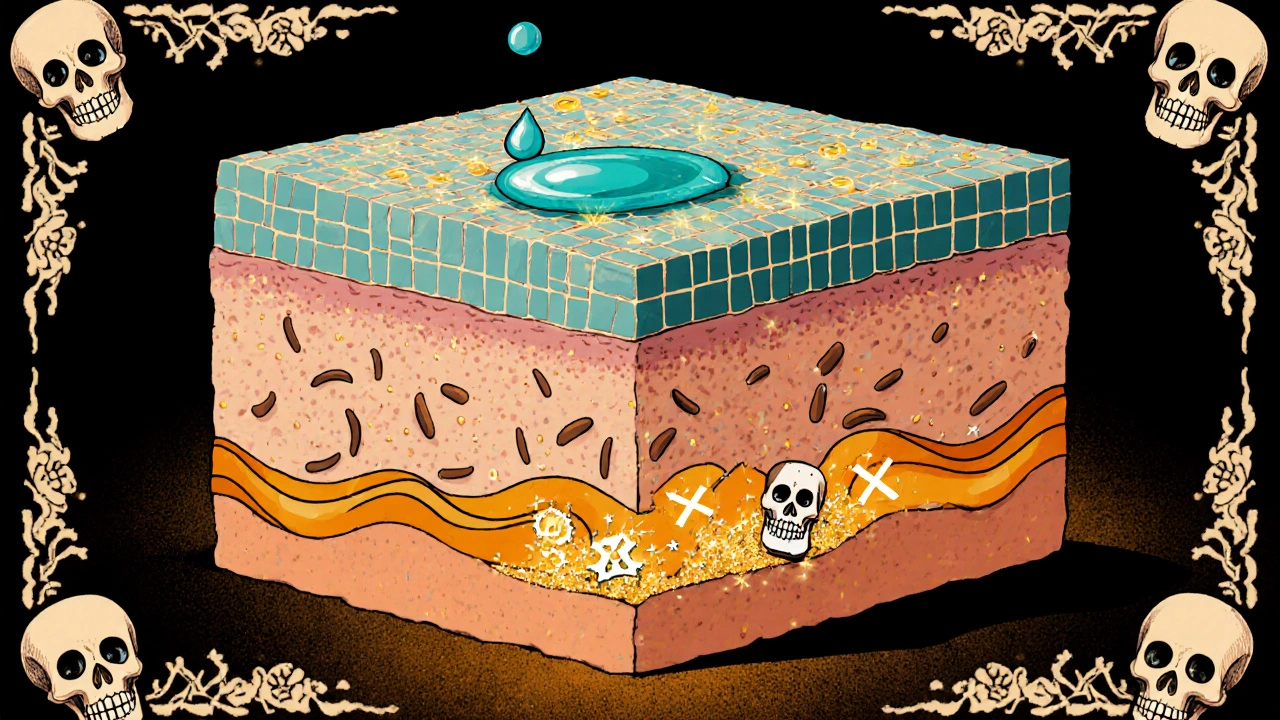
How Does a Topical Formulation Work?
Turning a solid pill into a cream isn’t just about mixing powder with water. Formulators must ensure the drug can cross the skin’s outer barrier - the stratum corneum - and reach the underlying tissues where pain lives. This is done by attaching meloxicam to lipophilic carriers, such as ethanol‑based gels or micro‑emulsions, that enhance permeation. Once applied, the drug diffuses into the dermis, where it can act on the COX‑2 enzymes in inflamed joints, tendons, or bursae.
Key pharmacokinetic differences appear:
- Local concentration: Skin levels can be 10‑20 times higher than plasma levels after a single dose, meaning you get a stronger effect where you need it.
- Systemic exposure: Blood concentrations are usually < 5 ng/mL, far below the threshold that triggers gastrointestinal or cardiovascular side effects.
- Onset: Pain relief can begin within 30‑60 minutes, compared with 1‑2 hours for oral meloxicam.
Benefits of Topical Meloxicam over Oral Forms
Choosing a skin‑applied product changes the risk‑benefit balance in several ways:
- Reduced GI risk: Oral NSAIDs irritate the stomach lining, leading to ulcers in up to 15 % of chronic users. The negligible systemic exposure of topical meloxicam dramatically lowers that risk.
- Fewer cardiovascular warnings: High‑dose oral NSAIDs have been linked to increased heart attacks. With topical use, plasma peaks stay well under the concerning range.
- Targeted therapy: If you have a knee that aches after a marathon, applying the cream directly to the joint concentrates the drug where it matters, without “wasting” it on other tissues.
- Convenient dosing: No need to swallow pills on an empty stomach. A pea‑size amount twice a day can be enough for many patients.
- Better compliance: Many patients report that a mild‑smelling gel is easier to incorporate into daily routine than a pill.
How to Use Topical Meloxicam Safely
Even though the product feels like a simple skin care item, it’s still a prescription medication. Follow these steps to keep it effective and safe:
- Clean the area: Wash the affected skin with mild soap, dry gently, and avoid applying over cuts or open wounds.
- Measure the dose: Most products come with a calibrated pump delivering 1 g (≈ 15 mg meloxicam). Use exactly the amount your doctor prescribes.
- Spread thinly: Rub the gel into the skin until it disappears. Do not cover with a bandage unless your doctor says it’s okay.
- Avoid sensitive regions: Do not use on the face, genitals, or mucous membranes.
- Watch for interactions: If you’re on other NSAIDs, anticoagulants, or certain antihypertensives, discuss potential additive effects with your pharmacist.
Typical regimens start with twice‑daily applications for the first week, then taper to once daily if pain improves. Most clinicians recommend a 4‑week trial before deciding whether to continue.
Comparing Topical Meloxicam with Other Topical NSAIDs
Diclofenac gel and ibuprofen cream have been on the market for years. Below is a quick side‑by‑side look at how they stack up.
| Feature | Topical Meloxicam | Diclofenac Gel (1 %) | Ibuprofen Cream (5 %) |
|---|---|---|---|
| COX Selectivity | COX‑2 selective | Non‑selective (COX‑1 & COX‑2) | Non‑selective (COX‑1 & COX‑2) |
| Typical Daily Dose | 30 mg (2 g × 15 mg/g) | 40 mg (4 g × 10 mg/g) | 75 mg (5 g × 15 mg/g) |
| Systemic Exposure | ~ 3‑5 ng/mL | ~ 8‑12 ng/mL | ~ 15‑20 ng/mL |
| Onset of Relief | 30‑60 min | 45‑90 min | 60‑120 min |
| Common Indications | OA, RA, localized musculoskeletal pain | OA, tendinitis, minor sports injuries | Back pain, minor sprains |
| Skin Irritation Rate | ~ 2 % | ~ 5 % | ~ 7 % |
Because meloxicam favors COX‑2, it tends to spare the protective COX‑1 activity in the stomach and kidneys, translating into fewer gastrointestinal complaints. That’s the main reason many clinicians see it as a “next‑generation” topical NSAID.
Potential Side Effects and Who Should Avoid It
Even with low systemic levels, some people still experience local or mild systemic reactions:
- Skin reactions: Redness, itching, or a mild rash at the site of application. If it spreads beyond the area or becomes painful, stop use and call your provider.
- Allergic dermatitis: Rare, but possible if you’re hypersensitive to meloxicam or to the cream’s excipients (e.g., ethanol, propylene glycol).
- Systemic NSAID effects: In very high‑dose or prolonged use, you could still see minor elevations in blood pressure or kidney markers, especially in patients with pre‑existing renal disease.
People who should generally avoid topical meloxicam include:
- Anyone with a known allergy to meloxicam or any component of the cream.
- Patients with severe liver impairment (dose adjustment required).
- Pregnant women in the third trimester - NSAIDs can affect fetal blood flow.
- Children under 12 years old, unless specifically prescribed off‑label.
Always discuss your full medication list with a pharmacist, especially if you take blood thinners, diuretics, or ACE inhibitors.
Frequently Asked Questions
Can I use topical meloxicam on a sunburn?
No. The cream is formulated for joints and soft tissue inflammation, not for burns. Applying it to a sunburn could increase irritation.
How long does a tube of topical meloxicam last?
A 30‑gram tube delivering 1 g per dose typically lasts about 2‑3 weeks when used twice daily. Your pharmacist can help you calculate exact usage based on your prescription.
Is it safe to combine topical meloxicam with oral ibuprofen?
Combining two NSAIDs increases the risk of kidney and GI complications. Most clinicians advise against using both at the same time unless a specialist has specifically ordered it.
Will the cream make my skin greasy?
Modern formulations use non‑oil‑based gels, so the finish is light and non‑greasy. It absorbs within minutes, leaving a barely noticeable residue.
Can I apply it before exercising?
Yes. Applying the gel 30 minutes before activity can pre‑empt inflammation. Just be sure the skin is dry before you start moving to avoid slipping.
Topical meloxicam represents a promising middle ground: strong anti‑inflammatory action where you need it, and a much gentler systemic footprint than traditional pills. If you struggle with joint pain, talk to your doctor about whether this new option fits your treatment plan.


Andrew Wilson
October 23, 2025 AT 22:30We all got a responsibility to read the fine print on every new med, especially when it’s a prescription‑strength NSAID turned into a cream. It’s not just a cute gel you slap on your knee and forget about; the drug still does serious work under the skin. If you ignore dosing instructions, you’re basically playing roulette with your gut and heart. So do yourself a favor and follow the doctor’s orders, no excuses.
Kristin Violette
October 27, 2025 AT 00:30Topical meloxicam illustrates a fascinating convergence of pharmacokinetic engineering and patient-centered therapeutics.
By leveraging the physicochemical properties of the COX‑2 selective molecule, formulators achieve transdermal permeation through the stratum corneum.
The incorporation of lipophilic carriers-such as ethanol‑based micro‑emulsions-exploits the Fickian diffusion gradient to concentrate drug at the inflamed synovial milieu.
Consequently, the local tissue concentration can exceed systemic plasma levels by an order of magnitude, which directly translates into amplified analgesic efficacy at the target site.
From a mechanistic perspective, the selective inhibition of COX‑2 attenuates prostaglandin E2 synthesis without compromising the gastroprotective prostaglandins generated by COX‑1.
This selectivity underpins the markedly reduced gastrointestinal adverse event profile observed in clinical trials.
Moreover, the diminished systemic exposure (<5 ng/mL) mitigates the cardiotoxic risk that has historically limited the chronic use of oral NSAIDs.
When initiating therapy, a calibrated 1 g dose delivering approximately 15 mg of meloxicam is recommended, applied to a clean, dry area of skin.
Patients should be counseled to avoid occlusion and to refrain from applying the gel to mucosal membranes, as barrier integrity influences percutaneous absorption.
The onset of analgesia, typically within 30–60 minutes, aligns with the rapid partitioning of the drug into the dermal interstitial fluid.
Comparatively, diclofenac and ibuprofen topical formulations exhibit non‑selective COX inhibition, which can account for their higher rates of cutaneous irritation.
In practice, the incidence of skin reactions with meloxicam gels hovers around 2 %, a figure that is clinically acceptable for most patients.
Nevertheless, clinicians must remain vigilant for signs of hypersensitivity, especially in individuals with a documented allergy to sulfonamide derivatives.
Long‑term safety data, while still accruing, suggest that renal function remains stable in patients without pre‑existing kidney disease.
In summary, topical meloxicam offers a compelling risk‑benefit calculus for osteoarthritis and localized musculoskeletal pain, provided that prescribing physicians adhere to the recommended dosing schedule and patient selection criteria.
Theo Asase
October 30, 2025 AT 03:30Wake up! The pharma overlords have engineered this so‑called ‘topical meloxicam’ to keep us dependent on their endless pipeline of pricey prescriptions. By masquerading as a harmless gel they can slip a COX‑2 inhibitor directly to our joints while we remain blissfully unaware of the hidden data suppression. They want us to think it’s safe because the systemic numbers are low, but they never disclose the long‑term dermal absorption studies that could reveal subtle endocrine disruption. This is not progress; it’s a stealthy assault on our autonomy, wrapped in a pretty tube.
Joey Yap
November 2, 2025 AT 06:30I get that new meds can feel intimidating, but the way this cream is designed actually respects the body’s own healing processes. By delivering meloxicam right where inflammation lives, it spares the stomach and reduces the systemic load. If you’re careful to follow the dosing guide and keep an eye on any skin irritation, it can be a gentle ally in managing joint pain. Think of it as a targeted patch rather than a blanket that covers everything.
Lisa Franceschi
November 5, 2025 AT 09:30Thank you for sharing your considerate perspective. It is indeed prudent to monitor the application site for any erythema or pruritus, particularly during the initial treatment phase. Should any adverse dermatologic response arise, discontinuation and consultation with a healthcare professional are advisable. Your balanced approach underscores the importance of patient education and vigilance.
Wilson Roberto
November 8, 2025 AT 12:30Folks, this is a great example of how modern pharmacology can align with daily routines. A pea‑size amount twice a day fits easily into a morning shower or bedtime ritual, and the non‑greasy gel disappears fast. Embrace the convenience, stay consistent, and you’ll likely notice reduced stiffness in weeks. Let’s keep moving forward with confidence.
Narasimha Murthy
November 11, 2025 AT 15:30While the data presented are compelling, one must scrutinize the study designs underpinning these claims. Many of the referenced trials are industry‑sponsored, potentially biasing outcome reporting. Moreover, the long‑term dermal safety profile remains under‑characterized, especially in populations with compromised skin barriers. A cautious, evidence‑based stance is warranted before wholesale adoption.
Samantha Vondrum
November 14, 2025 AT 18:30It is with great pleasure that I note the thoroughness of the presented information regarding topical meloxicam. The clinical implications are noteworthy, and the comparative tables provide valuable insight for prescribers. I commend the authors for their diligence in summarizing the pharmacologic nuances. 🙏
Kelvin Egbuzie
November 17, 2025 AT 21:30Oh sure, another “miracle” gel – because the big pharma has never tried to maximize profit by creating ever‑more niche products. 🙄 If you really trust the “low systemic exposure” hype, you’re ignoring decades of hidden data. Don’t be fooled by slick packaging.
Katherine Collins
November 21, 2025 AT 00:30Doen't really need a whole post for that.
Taylor Nation
November 24, 2025 AT 03:30I hear you. Simpler is often better, and if the short version works for you, that's what matters. Keep an eye on how your joints feel and adjust as needed.
Nathan S. Han
November 27, 2025 AT 06:30Picture this: a sleek tube of gel, the promise of targeted relief, and the patient poised on the brink of a new era of pain management. The drama unfolds as the meloxicam molecules breach the skin’s formidable barrier, marching straight to inflamed tissues. Their selective COX‑2 inhibition is a surgical strike that spares the stomach’s protective lining. The audience-your joints-responds with reduced swelling and a sigh of relief. Yet the true climax arrives when systemic side effects remain mere whispers in the background. It’s a story of precision, efficacy, and hope, all wrapped in a non‑greasy formula.
Ed Mahoney
November 30, 2025 AT 09:30Yeah, because we all love another gimmicky cream that pretends to be revolutionary while the real science is just old NSAID chemistry dressed up in a fancy bottle.
Brian Klepacki
December 3, 2025 AT 12:30Behold, the saga of the transdermal marvel! In a world where pills reign supreme, this gel emerges as the phoenix of analgesia, soaring above gastrointestinal perils. Its COX‑2 selective prowess dazzles like a star‑burst on a midnight canvas, leaving the meek COX‑1 behind. The formulation, a symphony of ethanol and lipids, conducts the meloxicam across the epidermal fortress with elegance. Witness the dawn of targeted therapy, where pain yields before the silken touch of modern pharmaceutics.
Shermaine Davis
December 6, 2025 AT 15:30Great info! I think this could help a lot of people who have joint pain and cant take pills.