Tumor Microenvironment (TME): A Practical Guide
The tumor microenvironment (TME) is the neighborhood around a cancer cell — and it often decides whether a tumor grows, stays quiet, or spreads. Knowing the main players and how they interact helps explain why some treatments work and others fail. This short guide gives you the essentials in plain language and tells you what matters most for patients and caregivers.
What's in the TME?
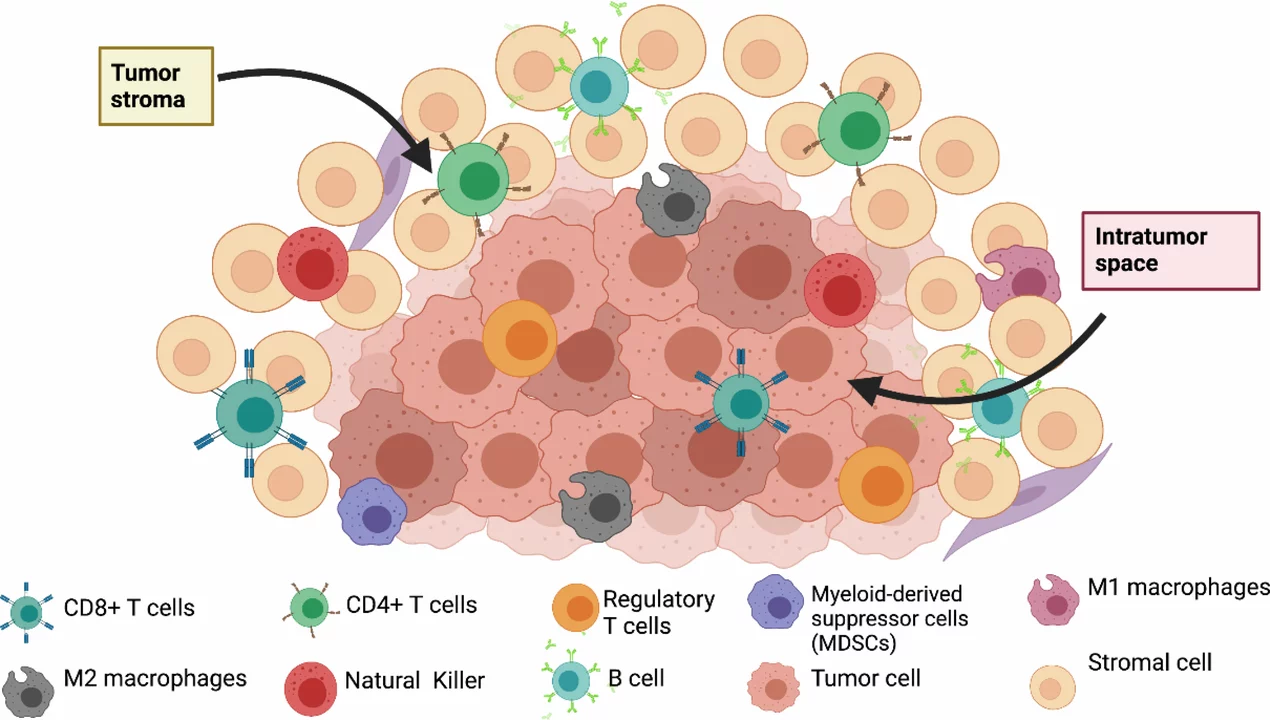
Think of the TME as a small ecosystem. It contains:
- Cancer cells: not all are the same; they evolve and behave differently even inside one tumor.
- Immune cells: T cells, macrophages, neutrophils and others. Some attack the tumor, some get co-opted to help it.
- Stromal cells: fibroblasts and other support cells that shape tissue structure and produce signaling molecules.
- Blood vessels and lymphatics: they supply oxygen and nutrients, but can also be abnormal and leaky.
- Extracellular matrix (ECM): the scaffold around cells. A dense ECM can block drugs and immune cells from reaching cancer.
- Chemical conditions: low oxygen (hypoxia), acidity, and altered nutrients change how cells behave and respond to therapy.
Why the TME changes treatment outcomes
If a tumor hides behind a suppressive immune environment or a dense ECM, drugs and immune cells can’t reach or kill cancer effectively. Hypoxia makes some therapies less effective and can drive more aggressive cancer traits. Tumors with lots of immune-suppressing cells often resist immunotherapy, while tumors with active, attacking immune cells respond better.
That’s why doctors now look beyond the cancer cell itself. Tests that profile immune cell presence, PD-L1 levels, or gene signatures from the TME can guide treatment choices. If you’re a patient, ask whether your tumor has been profiled for immune markers or if clinical trials considering the TME are an option.
How are researchers targeting the TME? There are practical strategies already in use or in trials:
- Immunotherapy: checkpoints inhibitors and CAR-T aim to reactivate immune cells suppressed by the TME.
- Anti-angiogenic drugs: normalize or block abnormal blood vessels to starve tumors or improve drug delivery.
- ECM-targeting approaches: enzymes or drugs that remodel the matrix to let drugs and immune cells in.
- Metabolic and hypoxia-targeting drugs: change the tumor’s chemical environment to make therapies work better.
Challenges remain. The TME is highly variable between patients and even within the same tumor. That means personalized profiling and combo therapies are often needed. If you’re talking with clinicians, ask about biomarker testing, possible combination treatments, and relevant trials focused on the microenvironment.
Understanding the TME gives you a clearer view of why some cancers respond quickly to therapy and others don’t. It’s not just about killing cancer cells — it’s about changing their neighborhood so cancer can’t hide anymore.