Epilepsy and Alcohol: Risks, Effects, and Safe Guidelines
Learn how alcohol impacts epilepsy, seizure risk, medication interactions, withdrawal effects, and safe drinking guidelines for better seizure control.
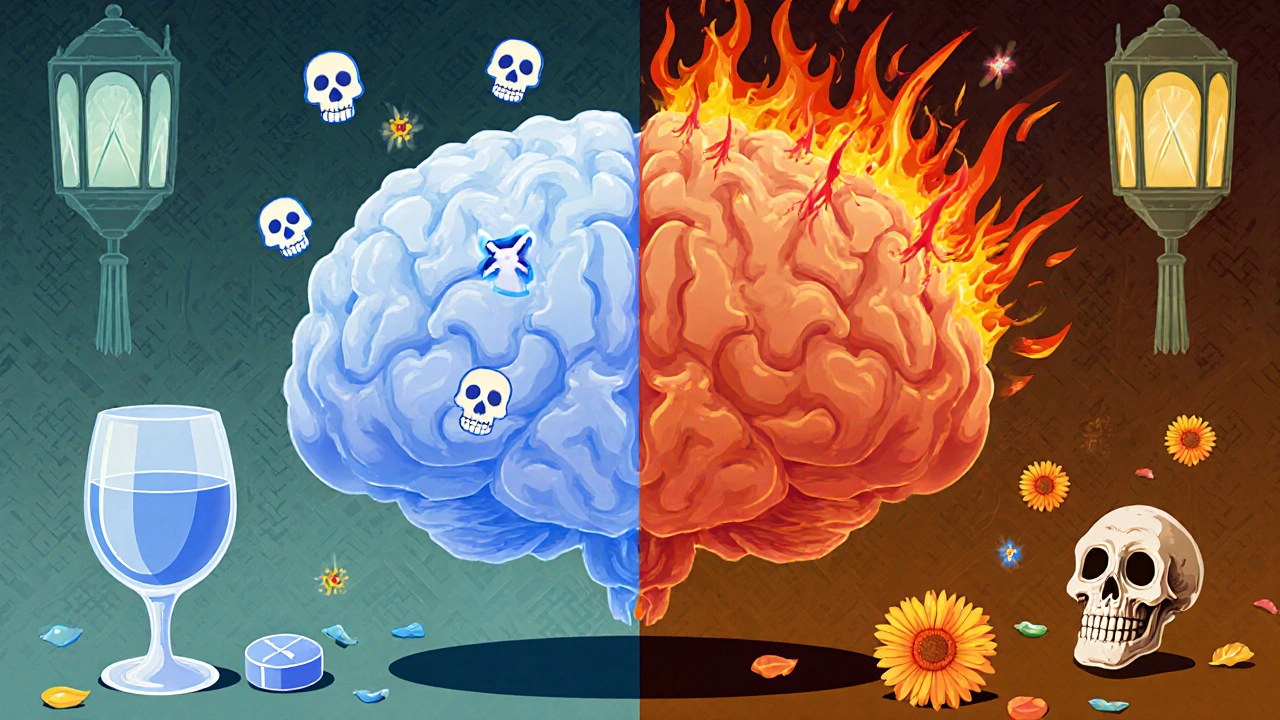
When dealing with epilepsy and alcohol, the combined effect of seizure disorders and alcohol consumption, many people wonder if a glass of wine is harmless or if it could trigger a seizure. The short answer is that alcohol can shift the delicate balance of brain excitability, especially for those already prone to seizures. Studies show that even moderate drinking can lower the seizure threshold, meaning the brain becomes more likely to fire unintentionally. This interaction matters because it influences daily choices, medication dosing, and long‑term health planning. Understanding the science helps you decide whether to sip, skip, or seek professional advice.
One major player is the seizure threshold, the level of electrical activity the brain can tolerate before a seizure occurs. Alcohol depresses certain brain pathways while simultaneously raising excitability in others, effectively pulling the threshold down. Another critical element is alcohol withdrawal, the set of symptoms that appear when regular drinking stops. Withdrawal can spike adrenaline and glutamate levels, creating a perfect storm for breakthrough seizures in people with epilepsy. Meanwhile, most antiepileptic drugs, medications used to control seizures are processed by the liver, and alcohol competes for the same metabolic pathways. This competition can raise drug levels, leading to side effects, or lower them, reducing seizure protection. Finally, liver metabolism, the body's process of breaking down substances like alcohol and medicines varies from person to person, meaning the same drink can affect two patients very differently. Together, these entities form a web of cause‑and‑effect: alcohol changes the seizure threshold, withdrawal adds stress, drug metabolism shifts, and the overall risk of a seizure goes up.
For practical management, keep epilepsy and alcohol discussions open with your neurologist. Many clinicians suggest limiting intake to a low‑risk level—often no more than one standard drink per day, and only on days when you’re seizure‑free. If you notice any change in seizure frequency after drinking, treat it as a warning sign and cut back. Adjustments to antiepileptic drug doses may be needed, especially if you have a history of liver issues. Some patients find that staying well‑hydrated, eating before drinking, and avoiding binge patterns reduce the likelihood of a seizure. Ultimately, the goal is to balance a social life with safety, and the articles below dive deeper into each of these topics, from medication interactions to withdrawal management and lifestyle tips.
Learn how alcohol impacts epilepsy, seizure risk, medication interactions, withdrawal effects, and safe drinking guidelines for better seizure control.