Atorvastatin — what it does and who it helps
Atorvastatin (brand name Lipitor) is a widely used statin that lowers LDL (“bad”) cholesterol and cuts heart attack and stroke risk. At higher doses it can reduce LDL by around 50% or more, which is why doctors often use it when cholesterol needs a big drop. If you’ve been told your LDL is high or you have cardiovascular risk factors, atorvastatin is one of the first medicines doctors consider.
How to take atorvastatin
Most people start atorvastatin at 10–20 mg once daily. Doctors may increase to 40–80 mg if more cholesterol lowering is needed. You can take it any time of day because atorvastatin stays active longer than some older statins, but taking it at the same time each day helps build a routine. If you miss a dose, take it when you remember unless it’s almost time for the next dose — don’t double up.
Don’t use atorvastatin if you’re pregnant or breastfeeding. If you plan pregnancy, talk with your doctor about stopping it beforehand. Also mention any liver problems or unexplained muscle pain before starting.
Side effects, monitoring, and interactions
Most people tolerate atorvastatin well, but common side effects include muscle aches, mild stomach upset, and small increases in liver enzymes. Serious muscle injury (rhabdomyolysis) is rare but possible, especially if you combine atorvastatin with certain drugs. Tell your doctor right away if you get severe muscle pain, weakness, or dark urine.
Before starting, doctors usually check liver tests and a baseline lipid panel. Follow-up lipid tests are common at 4–12 weeks to see how well it works, plus occasional liver tests afterward. If you get muscle symptoms, your doctor may order a CK (creatine kinase) test.
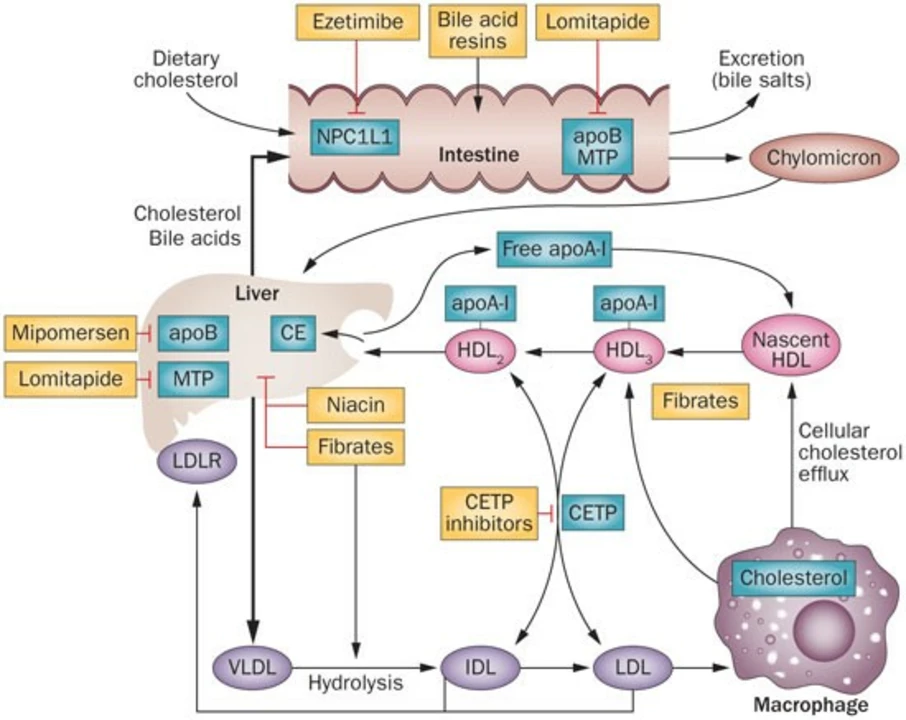
Atorvastatin is broken down by CYP3A4. That means some antibiotics (like clarithromycin), certain antifungals, HIV protease inhibitors, and grapefruit juice can raise atorvastatin levels and increase side effect risk. Combining atorvastatin with fibrates or high-dose niacin raises the chance of muscle problems too. Always tell your provider about every medicine and supplement you use.
What about alternatives? If statins aren’t suitable, options include ezetimibe (lowers cholesterol by blocking absorption), PCSK9 inhibitors (powerful injectable drugs), and lifestyle changes like diet, weight loss, and exercise. Some people explore supplements such as berberine or red yeast rice, but discuss these with your doctor because quality and effects vary.
Want practical tips? Keep a daily pill spot on your phone, report new muscle pain or jaundice, and bring a current med list to every visit. If you’re worried about side effects or want to compare options, ask your clinician for a plan that fits your health goals. Small steps—consistent meds, better food choices, and regular checks—add up to big heart benefits.