Epilepsy and Alcohol: Risks, Effects, and Safe Guidelines
Learn how alcohol impacts epilepsy, seizure risk, medication interactions, withdrawal effects, and safe drinking guidelines for better seizure control.
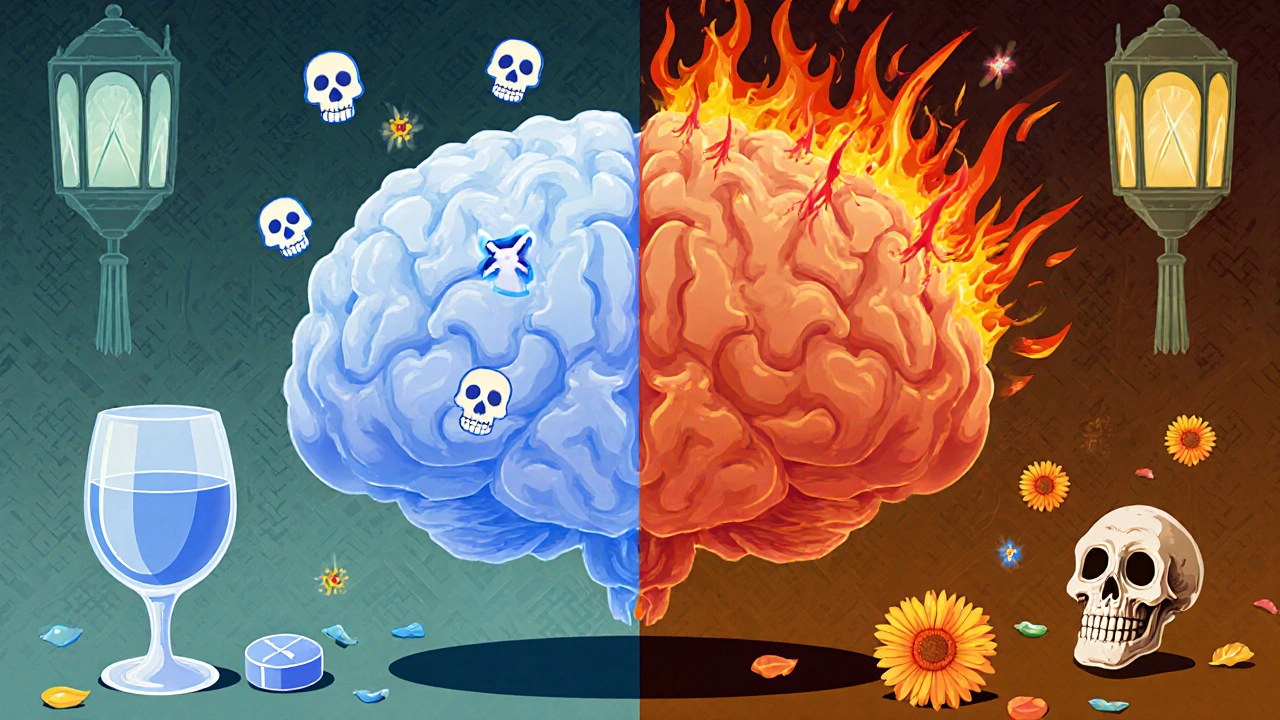
Alcohol Withdrawal Seizures are sudden convulsions that happen after abruptly stopping heavy alcohol use. Also known as AWS, they signal a rapid rebound of brain activity when alcohol’s calming effect disappears. Have you ever wondered why the brain goes into overdrive the moment someone quits drinking? The answer lies in how chronic alcohol reshapes neurotransmitters and how the nervous system reacts when that influence is gone.
Understanding Alcohol withdrawal is the collection of physical and psychological symptoms that appear when a regular drinker cuts back or stops completely is the first step. Symptoms range from mild tremors and anxiety to severe complications like seizures or delirium tremens. The timing matters: most seizures strike between 6 and 48 hours after the last drink, often before other severe signs appear. This window gives clinicians a short but critical period to intervene.
Risk factors shape who will experience AWS. Prior history of seizures, high daily alcohol intake, and a rapid reduction in drinking all raise the odds. Age and co‑existing medical conditions such as liver disease or electrolyte imbalance add extra danger. When you stack these factors, the brain’s excitatory pathways are primed for a burst, making seizure control a top priority.
The cornerstone of treatment is Benzodiazepine therapy that restores the brain’s inhibitory balance by enhancing GABA activity. Drugs like lorazepam or diazepam are given in doses that match the severity of symptoms. The goal isn’t just to halt a seizure; it’s to keep the nervous system from spiraling into delirium tremens, the most dangerous phase of withdrawal.
Monitoring electrolyte levels, especially magnesium and potassium, helps prevent seizure triggers. Intravenous fluids, thiamine supplementation, and careful blood pressure checks round out a comprehensive plan. Because seizures can recur, many clinicians keep patients under observation for at least 24‑48 hours after the first episode.
Delirium tremens represents the extreme end of the withdrawal spectrum. While not every seizure leads to DTs, the presence of a seizure dramatically raises that risk. DTs bring confusion, hallucinations, and autonomic instability, demanding intensive care. Recognizing the link early—seizure followed by escalating symptoms—lets providers escalate therapy before the patient slides into full‑blown delirium.
Patient education plays a huge role, too. People who understand that abruptly quitting can provoke seizures are more likely to seek medical detox rather than “cold turkey.” Gradual tapering, supervised by a healthcare professional, reduces the shock to the system and often prevents seizures altogether.
In practice, clinicians use standardized scales like the CIWA‑Ar (Clinical Institute Withdrawal Assessment for Alcohol) to gauge severity and adjust benzodiazepine dosing. The scale captures tremor intensity, anxiety, visual disturbances, and, crucially, the presence of seizures. A higher score prompts faster, larger medication doses to keep the brain stable.
Families also need clear guidance. If a loved one shows signs of a seizure—uncontrolled shaking, loss of consciousness, or tongue biting—call emergency services immediately. While waiting, keep the person safe from injury and avoid giving food or drink. Quick action can save lives and prevent the seizure from escalating into more severe withdrawal complications.
When you put all these pieces together—understanding the withdrawal process, spotting risk factors, using benzodiazepines wisely, and monitoring for delirium tremens—you build a solid defense against alcohol withdrawal seizures. Below you’ll find a curated list of articles that dive deeper into each of these topics, offering practical tips, medication comparisons, and real‑world case insights.
Explore the collection to see how specific drugs compare, learn self‑care strategies for withdrawal, and get detailed guidance on safe online pharmacy practices for related medications. The resources are designed to give you actionable knowledge whether you’re a patient, caregiver, or healthcare professional.
Learn how alcohol impacts epilepsy, seizure risk, medication interactions, withdrawal effects, and safe drinking guidelines for better seizure control.