Epilepsy and Alcohol: Risks, Effects, and Safe Guidelines
Learn how alcohol impacts epilepsy, seizure risk, medication interactions, withdrawal effects, and safe drinking guidelines for better seizure control.
When dealing with AED interactions, the way anti‑epileptic drugs influence each other and other medicines. Also known as anti‑epileptic drug interactions, they can alter seizure control, side‑effect risk, and overall health. Understanding them starts with knowing the anti‑epileptic drugs, medications like carbamazepine, phenytoin, levetiracetam, and valproate that keep seizures at bay. Each of these agents follows a metabolic path that can be boosted or blocked by enzyme inducers, substances that speed up liver enzymes such as CYP3A4, CYP2C9, and CYP2C19. When an inducer like carbamazepine meets a drug metabolized by the same enzyme—say oral contraceptives or certain antibiotics—the blood level of the second drug can drop, potentially causing treatment failure. The opposite happens with enzyme inhibitors (e.g., fluconazole, ritonavir) that raise AED concentrations, raising the chance of dizziness, ataxia, or toxic skin reactions. Because these shifts can happen quickly, clinicians often rely on therapeutic drug monitoring to keep levels in the sweet spot.
The importance of AED interaction knowledge stretches beyond seizure clinics. For instance, a pregnant patient on lamotrigine may need dose adjustments because hormonal changes affect metabolism, a principle mirrored in our post about Pregnancy Self‑Care. Similarly, the Tranexamic Acid for Post‑operative Bleeding article reminds us that antifibrinolytics can interfere with anticoagulant regimens, just as some AEDs clash with anticoagulants used after orthopedic surgery. When we compare Claritin vs. Other Allergy Meds, the discussion of antihistamine metabolism parallels how AEDs compete for the same cytochrome pathways. Even seemingly unrelated drugs like bupropion (covered in the Bupropion for Schizophrenia post) can act as mild enzyme inhibitors, subtly raising AED levels. Recognizing these cross‑topic links helps patients and providers anticipate side‑effects, avoid sub‑therapeutic dosing, and choose safer drug combinations.
Below you’ll find a curated set of articles that dive deep into specific drugs, dosing strategies, safety tips, and real‑world case examples. Whether you’re a clinician tweaking a regimen, a patient looking for practical advice, or a caregiver trying to understand why a new prescription changes how a seizure medication works, the collection offers actionable insights. Keep reading to see how each piece fits into the bigger picture of managing AED interactions safely and effectively.
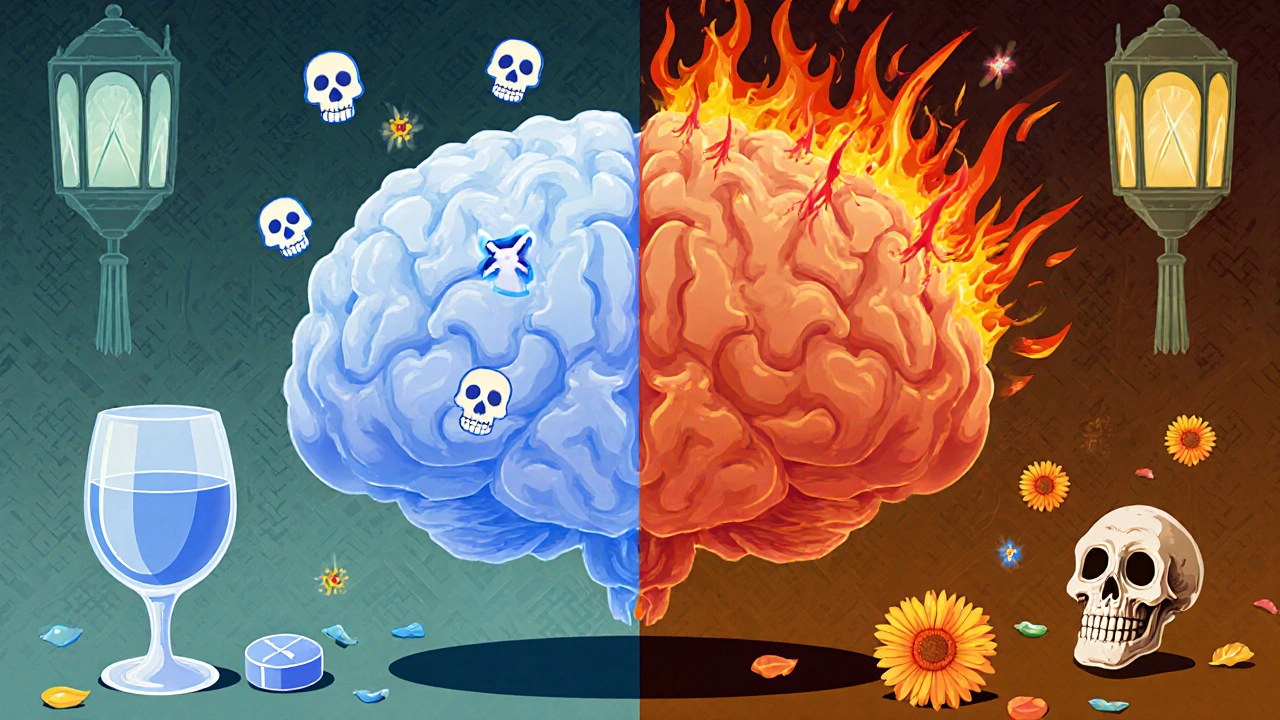
Learn how alcohol impacts epilepsy, seizure risk, medication interactions, withdrawal effects, and safe drinking guidelines for better seizure control.