Obesity Medication Dosing Calculator
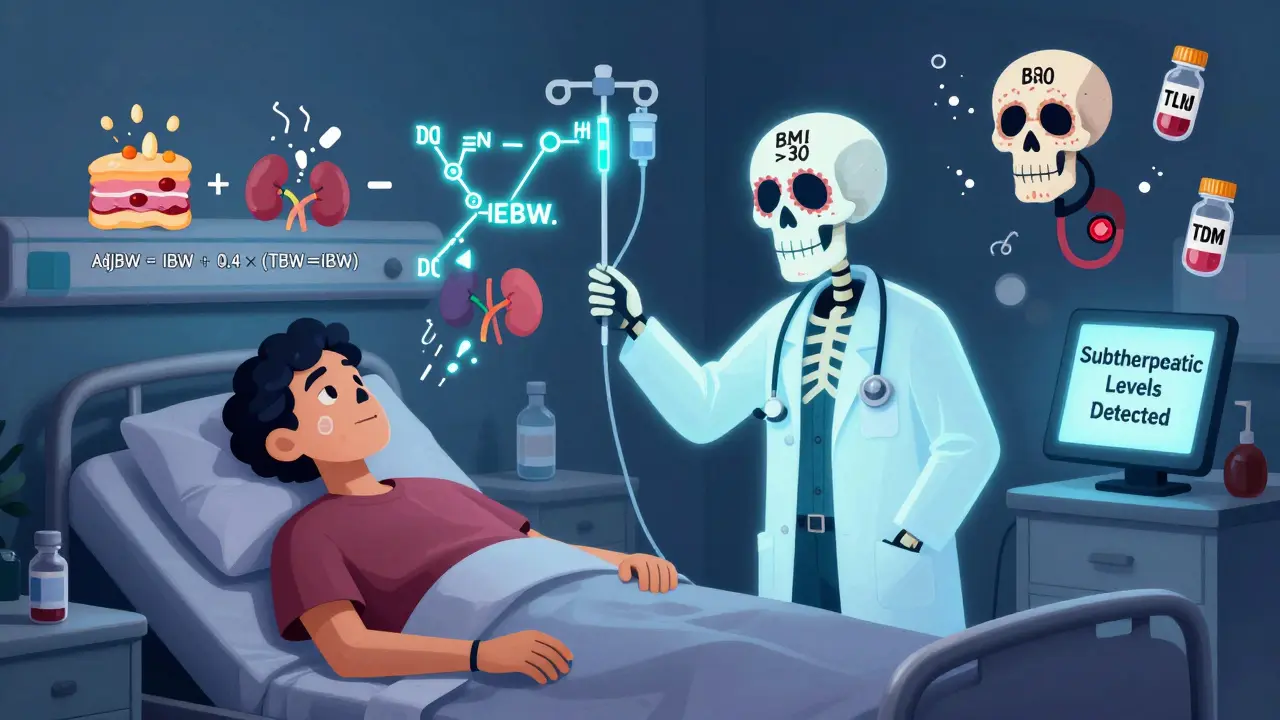
This tool helps calculate appropriate weight metrics for medication dosing in patients with obesity. Different drugs require different weight calculations based on whether they're fat-soluble or water-soluble.
Dosing Calculator
How to Use These Metrics
IBW (Ideal Body Weight): Use for water-soluble drugs (e.g., vancomycin, ceftriaxone) that don't accumulate in fat.
AdjBW (Adjusted Body Weight): Use for most antibiotics (e.g., ceftriaxone, tigecycline) when BMI >30.
LBW (Lean Body Weight): Use for fat-soluble drugs (e.g., diazepam, clindamycin) and anticoagulants.
Results
When you weigh more, your body doesn’t just carry extra fat-it changes how medicines work. For millions of people with obesity, taking the same dose as someone with a normal weight can mean the difference between treatment working and failing-sometimes dangerously so. Standard dosing guidelines were never built for bodies with high fat mass. Yet, nearly 40% of U.S. adults now have obesity, and that number keeps rising. Ignoring how fat affects drug behavior puts patients at risk of underdosing, overdosing, or both.
Why Obesity Changes How Drugs Work
Obesity isn’t just about weight. It’s about body composition. Fat tissue behaves differently than muscle, liver, or blood. It absorbs some drugs, blocks others, and changes how quickly the body clears them. A drug that dissolves easily in fat-like diazepam or clindamycin-can get trapped in fat tissue, spreading far beyond where it’s needed. That means the concentration in your bloodstream might be too low to fight an infection, even if you took the full dose. On the flip side, water-soluble drugs like antibiotics (cephazolin, vancomycin) don’t mix well with fat. They stay mostly in blood and fluid spaces. But obesity increases total blood volume and kidney function, so these drugs get flushed out faster. A standard 1g dose of ceftriaxone might be enough for someone who weighs 150 pounds, but for someone who weighs 300 pounds, it’s often too little. Studies show that 63% of obese patients on standard doses of ceftriaxone end up with drug levels too low to be effective. Then there’s protein binding. Many drugs attach to proteins in the blood to stay active. In obesity, those proteins can be stretched thin or altered, changing how much free drug is actually floating around to do its job. Add to that changes in liver enzyme activity and kidney filtration, and you’ve got a complex puzzle no standard chart can solve.Weight Metrics That Actually Matter
Doctors and pharmacists don’t just guess. They use specific calculations to estimate what body weight really matters for each drug. Here are the three most common:- Total Body Weight (TBW): Your actual weight on the scale. Often too high for water-soluble drugs and too low for fat-soluble ones.
- Ideal Body Weight (IBW): A calculated estimate of what your weight should be based on height and gender. Used for drugs that don’t accumulate in fat. For men: 50kg + 2.3kg per inch over 5 feet. For women: 45.5kg + 2.3kg per inch over 5 feet.
- Adjusted Body Weight (AdjBW): A hybrid. It takes IBW and adds 40% of the difference between TBW and IBW. Formula: AdjBW = IBW + 0.4 × (TBW − IBW). This is the go-to for many antibiotics in obese patients.
- Lean Body Weight (LBW): The weight of everything except fat. Harder to measure without scans, but critical for drugs like benzodiazepines or anticoagulants.
For example, when dosing enoxaparin (a blood thinner) for someone with a BMI over 40, studies show 40mg twice daily works for BMI 40-49.9, but if BMI hits 50 or higher, you need 60mg twice daily. Use the wrong number, and you risk clots or dangerous bleeding.
Antibiotics: Where the Biggest Risks Are
Antimicrobials are where obesity dosing errors are most common-and most dangerous. A 2024 study in Antimicrobial Agents and Chemotherapy found that up to 37% of obese patients on standard antibiotic doses experienced treatment failure. That means infections didn’t clear, leading to longer hospital stays, more surgeries, and higher death rates. Here’s what works based on current evidence:- Ceftriaxone: Use at least 2g daily for BMI >30. Standard 1g doses fail in over half of obese patients.
- Tigecycline: Use 100mg loading dose, then 50mg every 12 hours-no adjustment needed. New data suggests 200mg loading + 100mg every 12h for resistant infections.
- Colistin: Never dose by total weight. Use IBW, max 360mg colistin base activity per day. Obese patients have a 44% risk of kidney damage if overdosed.
- Voriconazole: Dosing by TBW leads to toxic levels in 39% of obese patients. Switching to AdjBW cuts that to 12%.
- Vancomycin: Always use therapeutic drug monitoring (TDM). Standard dosing often results in subtherapeutic levels, leading to MRSA treatment failure.
Therapeutic Drug Monitoring (TDM) isn’t optional anymore for many of these drugs. It means drawing blood to check actual drug levels in the bloodstream. If your vancomycin level is below 15 mcg/mL, you’re not getting enough. If it’s above 20, you’re risking kidney damage. TDM turns guesswork into precision.
When Dosing Rules Break Down
Some drugs have weird, arbitrary cutoffs that make no physiological sense. Apixaban, a blood thinner, uses a hard 85kg threshold: 5mg twice daily if under 85kg, 2.5mg if over. That’s a 50% drop at a single number. A patient weighing 84kg gets double the dose of someone at 86kg-even if their kidney function, age, and health are identical. Data shows this leads to a 47% higher bleeding risk just across that arbitrary line. Carvedilol, a beta-blocker, has the same issue. At 85kg, the dose jumps from 50mg to 100mg daily. No gradual increase. No adjustment for body fat. Just a cliff. Studies show these dichotomized dosing rules cause 32% more variation in drug levels than continuous, weight-based dosing like metoprolol, which scales smoothly with body weight. These aren’t just quirks-they’re safety hazards. And they persist because drug labels rarely update. Only 18% of FDA-approved drug labels contain any obesity-specific dosing guidance. Most doctors are left guessing.What Works in Real Hospitals
Some places have figured it out. At Stanford Health Care, pharmacists introduced AdjBW dosing for voriconazole in 2022. Before? Nearly 4 in 10 obese patients had toxic drug levels. After? That dropped to 12%. Dose adjustments fell by 57%. But it took eight weeks of training staff and rewriting protocols. UCSF saw similar results with ceftriaxone. After switching to 2g daily for obese patients, surgical site infections dropped from 14.2% to 8.7% in over 1,200 cases. But they had to fight pharmacy supply chains-hospitals weren’t stocking enough 2g vials. Mayo Clinic built an electronic alert into their system. When a patient with BMI >30 gets prescribed vancomycin, the EHR pops up: “Consider TDM. Standard dose likely insufficient.” Result? Subtherapeutic vancomycin levels dropped from 31% to 9%. Hospital stays for MRSA patients shortened by over two days. But many hospitals still don’t have protocols. A 2022 survey found only 37% of U.S. hospitals have formal obesity dosing guidelines. Even worse: 43% of internal medicine residents said they were confused about when to use IBW vs. TBW. One patient developed heparin-induced thrombocytopenia after being given too much enoxaparin because the resident used total body weight.
Getting Started: What You Need to Know
If you’re a clinician, here’s how to begin:- Calculate BMI: Weight (kg) ÷ height² (m²). Class I = 30-34.9, Class II = 35-39.9, Class III = ≥40.
- For every drug, ask: Is it fat-soluble or water-soluble?
- Use AdjBW for most antibiotics. Use IBW for drugs cleared by kidneys and not stored in fat.
- For anticoagulants, sedatives, and anticonvulsants, lean body weight is best if you can estimate it.
- Always check if TDM is recommended. For vancomycin, aminoglycosides, voriconazole, and linezolid-yes, it is.
- Use tools like the Clincalc Obesity Dosing Table (updated weekly) or DoseMe software.
Don’t rely on drug labels. They’re outdated. Don’t assume a 1g dose is enough. And never use total body weight for drugs like colistin or vancomycin without checking levels.
The Future: Precision Dosing Is Coming
The NIH just awarded $4.7 million to study how drug metabolism changes across the lifespan in obese patients. The FDA now requires obesity subgroup analysis in new drug trials. And by 2025, the IDSA plans to release a standardized BMI-based dosing algorithm. Long-term, the goal is precision dosing: combining body composition scans, genetic markers, and real-time TDM to tailor every dose. One expert predicts that within five years, we’ll use imaging to measure muscle and fat mass directly-and adjust doses like we adjust insulin for diabetes. Until then, the rule is simple: Obesity changes everything about how drugs behave. Standard doses are often wrong. If you’re treating someone with a BMI over 30, you’re not just treating a disease-you’re adjusting for their body’s unique chemistry. Get it right, and you save lives. Get it wrong, and you risk failure, toxicity, or both.Why can’t I just use total body weight for all medications?
Total body weight ignores fat vs. muscle. Fat doesn’t hold water-soluble drugs like antibiotics, so using TBW overdoses those. But fat absorbs fat-soluble drugs like diazepam or clindamycin, so TBW underdoses them. You need different weight metrics depending on the drug’s chemistry.
What’s the best way to calculate adjusted body weight?
Use this formula: Adjusted Body Weight = Ideal Body Weight + 0.4 × (Total Body Weight − Ideal Body Weight). For men: IBW = 50kg + 2.3kg per inch over 5 feet. For women: IBW = 45.5kg + 2.3kg per inch over 5 feet. This works well for most antibiotics in patients with BMI >30.
Is therapeutic drug monitoring really necessary for obese patients?
Yes, for several key drugs: vancomycin, aminoglycosides (like gentamicin), voriconazole, and linezolid. Studies show up to 60% of obese patients have drug levels outside the therapeutic range when dosed by weight alone. TDM prevents toxicity and treatment failure. It’s not optional-it’s standard of care.
Why do some drugs have sudden dose jumps at 85kg?
Those cutoffs are arbitrary, not scientific. They come from old clinical trial groupings, not pharmacokinetic data. Apixaban’s 85kg threshold leads to a 50% dose drop, but there’s no biological reason for it. Studies show this causes dangerous spikes in bleeding risk. Experts call these "clinically significant discontinuities" and recommend continuous dosing instead.
Where can I find reliable dosing guidelines for obese patients?
The most comprehensive free resource is the Clincalc Obesity Dosing Table (updated weekly). For antimicrobials, refer to the 2024 Castro-Balado review in Antimicrobial Agents and Chemotherapy. The IDSA and ASHP also publish annual guidelines. Avoid relying on drug labels-they’re outdated. Most don’t include obesity dosing.
Are there tools or apps that help with obesity dosing?
Yes. DoseMe (Australia) uses Bayesian modeling to predict drug levels based on weight, kidney function, and prior levels. Lexidrug and MediCalc include IBW and AdjBW calculators. Many academic hospitals use integrated EHR alerts. If your hospital doesn’t have one, advocate for it-implementation reduces errors by over 60%.


Laia Freeman
January 30, 2026 AT 05:35Frank Declemij
January 31, 2026 AT 21:15Andy Steenberge
February 2, 2026 AT 20:52Kacey Yates
February 4, 2026 AT 04:14Alex Flores Gomez
February 5, 2026 AT 21:15rajaneesh s rajan
February 7, 2026 AT 14:19Pawan Kumar
February 7, 2026 AT 16:38DHARMAN CHELLANI
February 8, 2026 AT 19:23kabir das
February 9, 2026 AT 09:39Keith Oliver
February 11, 2026 AT 04:11LOUIS YOUANES
February 12, 2026 AT 19:40ryan Sifontes
February 14, 2026 AT 09:56Laura Arnal
February 14, 2026 AT 14:31paul walker
February 14, 2026 AT 17:05