Angioedema Type Identifier
Medication-Induced Angioedema Assessment
This tool helps you determine if your swelling might be medication-induced angioedema and whether it's likely histamine-mediated or bradykinin-mediated. Your treatment depends on this distinction.
Results
Swelling in your lips, tongue, or throat isn’t just uncomfortable-it can kill you in minutes. When it’s caused by a medication you’ve been taking for months or even years, you might never see it coming. This isn’t a rare allergy story. It’s a quiet, deadly side effect hiding in plain sight, especially with common drugs like blood pressure pills. Angioedema from medications is one of the most under-recognized emergencies in primary care, and misdiagnosis leads to delayed treatment, repeated hospital visits, and sometimes death.
What Exactly Is Medication-Induced Angioedema?
Angioedema isn’t a rash. It’s deep swelling beneath the skin or mucous membranes-think lips, tongue, throat, intestines, or limbs. Unlike hives, which sit on top of the skin, this swelling pushes up from below, often without redness or itching. It can start subtly, like a feeling of fullness in your lips, then rapidly turn into something terrifying: your tongue feels thick, your voice changes, or you can’t swallow. If it hits your airway, breathing becomes impossible.
There are two main types, and they need completely different treatments. One is caused by histamine release-like a classic allergic reaction to penicillin or aspirin. The other is driven by bradykinin, a chemical that causes blood vessels to leak fluid into tissues. This second type is what happens with ACE inhibitors, the most common drug culprit. And here’s the catch: epinephrine, antihistamines, and steroids don’t work on bradykinin-mediated angioedema. Giving them delays real treatment and wastes precious time.
Which Medications Cause It?
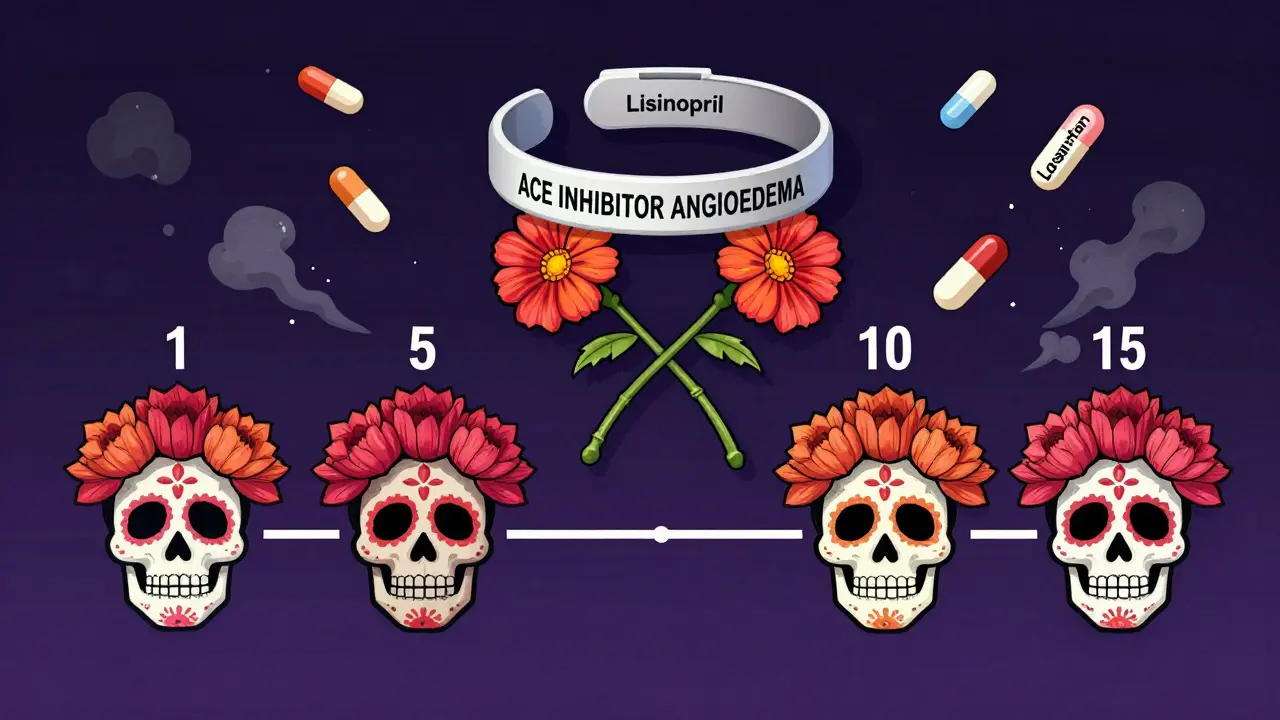
ACE inhibitors are the biggest offender. These include lisinopril, enalapril, ramipril, and benazepril-medications prescribed to over 50 million Americans for high blood pressure and heart failure. About 0.1% to 0.7% of people on these drugs develop angioedema. But the risk jumps to 2.2% in African-American patients and is higher in women. And it doesn’t just happen early. Half of cases occur after the first year of use. Some people take it for 10 years before swelling hits.
Other common triggers include:
- Angiotensin receptor blockers (ARBs) like losartan or valsartan-up to 50% of people who had ACE inhibitor angioedema will get it again if switched to an ARB
- NSAIDs like ibuprofen or naproxen
- Aspirin
- Penicillin and other antibiotics
- Some blood pressure meds like calcium channel blockers (less common)
It’s not just about the drug name-it’s about the mechanism. If a drug affects the bradykinin pathway, you’re at risk. That’s why switching from an ACE inhibitor to an ARB isn’t a safe workaround. Both mess with the same system.
Why Is This So Dangerous?
Because it can look like a simple allergic reaction. Patients go to the ER with swollen lips. The doctor gives them Benadryl and steroids. They feel better. They go home. A week later, it happens again. Then again. By the third time, they’re in the ICU with a blocked airway. A 2019 Mayo Clinic study of 1,200 cases found that 68% had visited the ER at least once before being correctly diagnosed. Twenty-two percent needed intubation.
Dr. Marcus Maurer, a leading expert in allergy and dermatology, says voice changes, stridor (a high-pitched breathing sound), sudden difficulty breathing, or fainting are red flags. Abdominal pain from intestinal swelling is also common and often mistaken for appendicitis or food poisoning. If you’re on an ACE inhibitor and suddenly have unexplained swelling or belly pain, don’t wait. Go to the ER.
And here’s the worst part: many doctors still don’t know. A 2022 survey by the American College of Physicians found only 45% of primary care physicians correctly identified ACE inhibitors as the #1 drug cause of angioedema. That means patients are getting the wrong treatment over and over.

How to Tell the Difference: Histamine vs. Bradykinin
Knowing which type you have changes everything.
| Feature | Histaminergic (Allergic) | Bradykinin-Mediated (Drug-Induced) |
|---|---|---|
| Onset | Minutes after taking drug | Hours to days after starting or even years later |
| Itching or hives | Common | Rare |
| Response to antihistamines | Yes | No |
| Response to epinephrine | Yes | No |
| Response to steroids | Yes | No |
| Typical triggers | Penicillin, NSAIDs, aspirin | ACE inhibitors, ARBs |
| Duration | 24-48 hours | 2-5 days |
If you have swelling without hives or itching, especially if you’re on a blood pressure pill, assume it’s bradykinin-mediated until proven otherwise. That means skipping the usual allergy meds and heading straight to emergency care.
What Happens in the Emergency Room?
If you’re having airway swelling, time is everything. You have 30 to 60 minutes before the situation becomes critical. The first thing they’ll do is check your airway. If it’s narrowing, they may need to intubate or perform an emergency tracheostomy.
For histamine-driven angioedema, treatment is straightforward: epinephrine shot, antihistamines, and steroids. But for bradykinin-mediated cases-like from ACE inhibitors-those won’t work. Instead, they’ll use:
- C1-inhibitor concentrate (Berinert, Cinryze)
- Icatibant (Firazyr)-a shot that blocks bradykinin receptors
- Ecallantide (Kalbitor)-a kallikrein inhibitor
These drugs are expensive and not always in every ER, but they’re life-saving. That’s why awareness matters. Some hospitals now have angioedema protocols that include keeping icatibant on hand for high-risk patients.
What Should You Do If You Suspect It?
If you’re on an ACE inhibitor or ARB and notice any swelling-lips, tongue, throat, face, hands, feet, or even unexplained belly pain-stop the medication immediately. Call 911 or go to the ER. Don’t wait. Don’t take an antihistamine and hope it goes away. That could cost you your airway.
Once you’re stable, see an allergist or immunologist. They’ll help you figure out what caused it and how to avoid it in the future. You’ll need a medical alert bracelet and a written action plan. If you’ve had one episode, you’re at high risk for another.
And never, ever restart the drug-even if you were told it was "just allergies." That’s how people lose teeth from tongue swelling or end up on a ventilator.
Long-Term Management and Prevention
If you’ve had medication-induced angioedema, you need a new treatment plan for your blood pressure. Safe alternatives include calcium channel blockers (like amlodipine), diuretics, or beta-blockers-none of which trigger bradykinin buildup. Your doctor should review all your meds, including over-the-counter painkillers.
For those with recurrent episodes, newer drugs like sebetralstat (approved in 2023) show promise for bradykinin-related swelling, even if it’s drug-induced. Research is ongoing, but early data suggests these oral treatments could reduce attacks by 70% or more.
Patients who’ve been misdiagnosed often say the same thing: "I wish someone had told me sooner." One Reddit user, u/AngioWarrior, shared: "My doctor kept telling me it was just allergies for 3 years while I was on lisinopril-lost 2 teeth from tongue swelling before they finally connected the dots."
That’s the real tragedy-not the swelling itself, but the delay in recognizing it. With better education, we could prevent most of these cases.
What’s Being Done to Fix This?
There’s progress. The 2023 International WAO/EAACI guidelines now include clear diagnostic criteria to distinguish between histamine and bradykinin types. Hospitals in major cities are starting to train ER staff on angioedema protocols. The FDA has had black box warnings on ACE inhibitors since 1999, but those warnings don’t reach most patients.
The global market for angioedema treatments is growing fast-projected to hit $2.4 billion by 2028-but most of that money goes to rare hereditary cases. Drug-induced cases still lack targeted therapies and public awareness. The European Academy of Allergy predicts a 30% drop in deaths by 2028-if doctors learn to recognize the signs.
Until then, the best defense is knowledge. If you’re on a blood pressure pill and suddenly feel like your mouth is full of cotton, don’t ignore it. Don’t assume it’s allergies. Don’t wait for the swelling to get worse. Your life depends on acting fast.
Can you get angioedema from blood pressure meds even after years of taking them?
Yes. While some cases happen within the first week, half of all ACE inhibitor-induced angioedema cases occur after the first year, and some appear after 5, 10, or even 15 years of use. There’s no safe window-anyone on these drugs can develop it at any time.
If I had angioedema from lisinopril, can I take losartan instead?
No. Losartan is an ARB, and it works on the same biological pathway as ACE inhibitors. Up to 50% of people who had angioedema from an ACE inhibitor will have it again if switched to an ARB. You need a completely different class of blood pressure medication, like a calcium channel blocker or diuretic.
Do antihistamines help with drug-induced angioedema?
Only if it’s histamine-mediated, like from penicillin or NSAIDs. If it’s from an ACE inhibitor or ARB, antihistamines won’t work. Giving them delays the right treatment and can be dangerous. If swelling happens without hives or itching, assume it’s bradykinin-related and seek emergency care immediately.
Is angioedema from medication hereditary?
No. Medication-induced angioedema is not inherited. It’s caused by how the drug affects your body’s chemistry. However, hereditary angioedema (HAE) is a separate genetic condition that can look similar. If you have recurrent episodes without a clear drug trigger, you may need testing for C1-inhibitor deficiency.
Should I carry an EpiPen if I’m on an ACE inhibitor?
Not unless you’ve had a confirmed allergic reaction to something else, like peanuts or penicillin. An EpiPen won’t help with ACE inhibitor angioedema. Carrying one might give you a false sense of security. Instead, know the signs, stop the drug immediately if swelling starts, and go to the ER. Keep a list of your meds and a note saying "suspected ACE inhibitor angioedema" in your wallet.
How long does medication-induced angioedema last?
Mast cell-mediated (allergic) swelling usually lasts 24-48 hours. Bradykinin-mediated swelling from ACE inhibitors can last 2-5 days. Even after swelling goes down, the risk of recurrence remains high if you’re re-exposed to the drug. Never restart the medication without consulting a specialist.


jeremy carroll
December 15, 2025 AT 19:30Alexis Wright
December 16, 2025 AT 16:51Wade Mercer
December 17, 2025 AT 06:39Daniel Thompson
December 17, 2025 AT 16:30Sarthak Jain
December 18, 2025 AT 11:36Tim Bartik
December 20, 2025 AT 05:22Sinéad Griffin
December 21, 2025 AT 12:20Thomas Anderson
December 21, 2025 AT 23:24Edward Stevens
December 23, 2025 AT 19:15Daniel Wevik
December 24, 2025 AT 07:21Rich Robertson
December 26, 2025 AT 00:59