Think you have a bad case of gas or cramps after eating? Maybe it’s just IBS. But what if it’s something more serious - something that can damage your intestines for life? You’ve probably heard people use IBS and IBD interchangeably, but they’re not the same. One is a dysfunction of how your gut works. The other is actual physical damage inside your digestive tract. Confusing them can delay treatment, worsen symptoms, or even put your health at risk.
IBS: Your Gut Is Working, But It’s Misfiring
IBS - Irritable Bowel Syndrome - doesn’t show up on scans, blood tests, or colonoscopies. Your intestines look perfectly normal. But you still feel terrible: cramps, bloating, diarrhea, constipation, or a mix of both. It’s not in your head. It’s in your nerves and muscles.
The Rome IV criteria, the gold standard used by doctors since 2016, says IBS means you’ve had abdominal pain at least once a week for three months, linked to bowel movements or changes in stool. About 76% of people with IBS report constant bloating. Nearly half see mucus in their stool. Symptoms flare after meals, during stress, or around your period - especially if you’re a woman, since 65% of IBS cases are in women.
Here’s the key: no inflammation. No ulcers. No bleeding. No damage you can see. That’s why doctors diagnose IBS by ruling everything else out. If your blood work is clean, your colonoscopy shows no swelling or sores, and you don’t have weight loss or fever, then IBS is likely the answer.
It’s frustrating because you can’t prove it with a test. But that doesn’t make it less real. People with IBS often say they’d give up coffee, their phone, or even sex to be free of the pain. It messes with sleep, work, and relationships. But here’s the good news: IBS doesn’t turn into cancer. It doesn’t cause bowel obstructions. It doesn’t shorten your life.
IBD: Your Gut Is Actually Sick
IBD - Inflammatory Bowel Disease - is a group of conditions where your immune system attacks your digestive tract. The two main types are Crohn’s disease and ulcerative colitis. Both cause chronic inflammation. And that inflammation doesn’t just hurt - it destroys.
In ulcerative colitis, the inner lining of your colon becomes raw and ulcerated. In Crohn’s, inflammation can happen anywhere from mouth to anus, and it eats through all layers of the bowel wall. That’s why IBD patients often have blood in their stool - 92% of ulcerative colitis patients do at diagnosis. Black, tarry stools? That’s internal bleeding higher up. Unexplained weight loss? Common. Fever? Yes. Joint pain, eye redness, skin rashes? Those are signs your immune system is on fire beyond your gut.
Doctors don’t guess at IBD. They see it. A colonoscopy will show red, bleeding, ulcerated tissue. Biopsies confirm inflammation under the microscope. Blood tests show high CRP levels - over 5 mg/L, when normal is under 3. Stool tests reveal calprotectin above 250 µg/g, a clear sign of gut inflammation. MRI scans find strictures, fistulas, or abscesses. In 33% of Crohn’s patients, scar tissue narrows the intestine within 10 years. In 17%, abnormal tunnels (fistulas) form between organs.
IBD doesn’t just cause discomfort - it causes complications. After 10 years of full-colon ulcerative colitis, your risk of colorectal cancer jumps by 2% each year. Toxic megacolon - a life-threatening swelling of the colon - happens in 2-4% of severe cases. IBD can require surgery, stoma bags, or long-term immunosuppressants.
The Big Difference: Damage vs. Dysfunction
Here’s the simplest way to tell them apart: IBS is a malfunction. IBD is a breakdown.
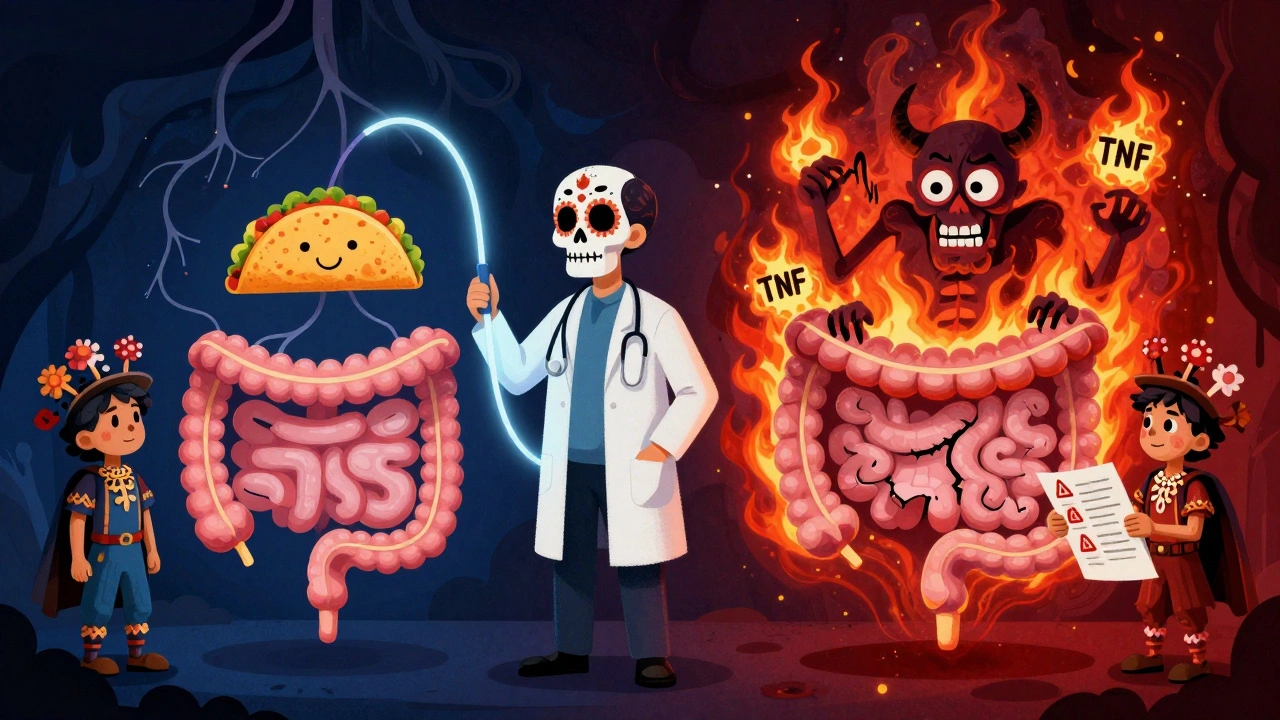
With IBS, your gut is like a miswired thermostat. It overreacts to normal signals. Food moves too fast or too slow. Nerves scream pain when there’s no injury. But the structure? Intact.
With IBD, your gut is like a house on fire. The walls are burning. The pipes are leaking. The damage is visible, measurable, and progressive. You can’t fix IBD by eating differently alone. You need drugs that shut down your immune system’s attack.
That’s why symptoms like blood in stool, fever, or sudden weight loss are red flags for IBD - not IBS. If you’re losing weight without trying, or your stool looks like red wine, see a doctor immediately. Those aren’t IBS signs. They’re signs your gut is being eaten from the inside.
How They’re Diagnosed - And Why It Matters
IBS diagnosis is a process of elimination. Your doctor checks for anemia, infections, celiac disease, and IBD. If all tests come back normal and your symptoms match Rome IV criteria, you get an IBS diagnosis. No biopsy needed. No imaging required. Just a clear pattern of symptoms and the absence of alarm signs.
IBD diagnosis is invasive by design. You need a colonoscopy with tissue samples. Blood tests for CRP and calprotectin. Sometimes an MRI or CT scan to see deeper layers of the bowel. You’re not just being checked - you’re being scanned for damage.
One mistake doctors see often: assuming IBS because no one found inflammation yet. But early Crohn’s can be subtle. If symptoms persist, repeat testing is critical. Delayed IBD diagnosis means more damage, more surgeries, and higher cancer risk.
Treatment: Calming Nerves vs. Stopping Inflammation
IBS treatment focuses on managing signals. No cure, but plenty of relief.
- The low-FODMAP diet cuts fermentable carbs that trigger gas and bloating - it works for 76% of people.
- Low-dose antidepressants like amitriptyline calm overactive gut nerves and reduce pain in 60% of patients.
- Medications like eluxadoline help control diarrhea in IBS-D by slowing bowel movement speed.
- Probiotics, peppermint oil, and stress reduction (CBT, mindfulness) also help many.
IBD treatment fights fire with fire. You need drugs that suppress your immune system.
- Corticosteroids like prednisone calm acute flares - but you can’t stay on them long due to bone loss, diabetes, and mood swings.
- Biologics like infliximab block TNF-alpha, a key inflammation trigger. About half of Crohn’s patients go into remission within 14 weeks.
- Vedolizumab targets gut-specific inflammation and helps nearly half of ulcerative colitis patients stay in remission after a year.
- Surgery may be needed for strictures, fistulas, or cancer risk.
Important note: You can have both IBS and IBD. Studies show 22-35% of IBD patients in remission still have IBS-like symptoms. That doesn’t mean their IBD came back. It means their gut nerves are still hypersensitive after the inflammation cooled down.

What You Should Do If You’re Unsure
Don’t self-diagnose. Don’t assume it’s IBS because you don’t have blood in your stool. And don’t ignore symptoms just because a doctor said "it’s probably IBS."
Here’s your checklist:
- Got blood in stool? Go to a doctor now. Not next week. Now.
- Lost weight without trying? Get tested. This isn’t normal.
- Have a fever with belly pain? That’s IBD territory.
- Family history of IBD or colon cancer? Push for more testing.
- Diarrhea or constipation for months with no alarm signs? Try IBS protocols - diet, stress, probiotics.
If you’ve been told you have IBS but still feel worse after a year of diet changes and supplements, ask for a repeat colonoscopy or calprotectin test. Symptoms can change. Conditions can evolve.
IBS is manageable. IBD is treatable. But only if you know which one you have.
Can IBS turn into IBD?
No. IBS cannot turn into IBD. They are completely different conditions. IBS is a functional disorder - your gut functions abnormally but has no structural damage. IBD is an inflammatory disease with visible tissue damage. Major medical organizations like the Crohn’s & Colitis Foundation and the CDC confirm there is no progression from IBS to IBD. However, some people with IBD may develop IBS-like symptoms during remission, which is a separate issue.
Does IBD always cause bleeding?
Not always, but it’s very common - especially in ulcerative colitis, where 92% of patients have blood in their stool at diagnosis. In Crohn’s disease, bleeding is less frequent but still occurs in about 30% of cases, especially when the colon is involved. Blood in stool is a major red flag for IBD and should never be ignored. It’s not a normal part of IBS.
Can stress cause IBD?
Stress doesn’t cause IBD, but it can trigger flares. IBD is an autoimmune disease driven by genetics and immune dysfunction. You can’t catch it or stress yourself into it. But if you already have IBD, high stress levels can make symptoms worse and increase the chance of a flare. Managing stress won’t cure IBD, but it helps you stay in remission longer.
Is IBS a mental health issue?
No. IBS is a real physical disorder of the gut-brain axis - the communication line between your digestive system and your nervous system. It’s not "all in your head," even though emotions can trigger symptoms. The pain, bloating, and bowel changes are caused by abnormal muscle contractions and heightened nerve sensitivity in the gut. Many people with IBS have normal brain scans and perfectly healthy mental health. It’s a physiological problem, not a psychological one.
Can you have both IBS and IBD at the same time?
Yes. About 22-35% of people with IBD who are in remission still meet the criteria for IBS. That means their gut inflammation is under control, but their nerves remain overly sensitive. This is called "post-inflammatory IBS." It’s not a sign that IBD is returning - it’s a lingering functional issue after the inflammation healed. Treatment for this combo often combines IBD maintenance meds with IBS symptom management like low-FODMAP diet or gut-directed therapy.
What’s the best test to tell IBS from IBD?
The most reliable test is a colonoscopy with biopsy, combined with blood and stool tests. Blood tests check for elevated CRP (a marker of inflammation), and stool tests measure calprotectin - a protein released by white blood cells in inflamed guts. Calprotectin above 250 µg/g strongly suggests IBD. Normal levels make IBD unlikely. If your colonoscopy shows ulcers, swelling, or abnormal tissue, it’s IBD. If everything looks normal and your symptoms match Rome IV criteria, it’s IBS.
Final Takeaway
IBS and IBD both wreck your quality of life. But only one can wreck your intestines. If you’re tired of guessing, get tested properly. Don’t settle for "it’s probably IBS" if you have warning signs. Blood in stool? Weight loss? Fever? Don’t wait. Get the right diagnosis - because the treatment, the risks, and the future depend on it.


Louis Llaine
December 7, 2025 AT 06:40So let me get this straight - if I eat a burrito and my gut rebels, it’s not because I’m a walking gas chamber, it’s my ‘nerves misfiring’? Cool. So next time I’m in pain, I’ll just tell my colon to chill out and maybe it’ll stop acting like a toddler with a juice box. 😴
Jane Quitain
December 8, 2025 AT 21:08YALL I JUST FOUND OUT I MIGHT HAVE IBS AND I’M SO RELIEVED BECAUSE I THOUGHT I WAS DYING 😭 I’VE BEEN EATING BANANAS AND DRINKING PEPPERMINT TEA AND I FEEL LIKE A NEW PERSON!! YOU GOT THIS!! 💪🌸
Ernie Blevins
December 10, 2025 AT 02:29IBS is just lazy gut syndrome. People want a diagnosis so they can stop trying. You don’t need a test to know if you’re eating garbage. Stop blaming your nerves and start blaming your diet. Also, probiotics are a scam. Your gut doesn’t need a spa day, it needs discipline.
Nancy Carlsen
December 10, 2025 AT 22:08OMG this post is a GAME CHANGER 🌟 I’ve been scared to go to the doctor for years but now I know blood in my stool isn’t ‘just hemorrhoids’ - I’m booking my colonoscopy TOMORROW!! Thank you for making this so clear!! 🤗❤️
Jennifer Anderson
December 11, 2025 AT 21:27i just read this and realized i’ve been treating my ibs like it’s a phase… but it’s been 3 years. i’m gonna try the low fodmap thing. also, i never knew stress could make it worse but it totally makes sense now. thanks for sharing!! 🙏
Sadie Nastor
December 11, 2025 AT 22:10Reading this felt like someone finally understood me. I’ve had both IBD and IBS symptoms at different times, and the confusion made me feel crazy. Knowing they can coexist… it’s a relief. You’re not alone if you’re tired, bloated, and still scared to eat pizza. We got this. 🌿
Nicholas Heer
December 12, 2025 AT 17:06THEY DON’T WANT YOU TO KNOW THIS BUT IBD IS A BIG PHARMA SCAM TO SELL BIOLICS. THEY MAKE YOU THINK YOU NEED IMMUNOSUPPRESSANTS WHEN REALLY YOU JUST NEED TO CLEANSE YOUR COLON WITH APPLE CIDER VINEGAR AND STAY AWAY FROM THE GOVERNMENT’S GMO CORN. I’VE BEEN CURED BY A GURU IN ARIZONA. TRUST THE PROCESS. 🇺🇸🔥
Sangram Lavte
December 13, 2025 AT 04:12This is very well explained. I have a cousin with Crohn’s and I never understood the difference between IBS and IBD until now. The part about calprotectin and colonoscopy made it clear. Thank you for writing this with such care. It helps people like me who are trying to support loved ones.
Oliver Damon
December 14, 2025 AT 06:34The real distinction here isn’t just clinical - it’s ontological. IBS represents the body’s attempt to communicate distress through dysfunction, while IBD is the body’s collapse into structural failure. One is a signal, the other is a system breach. We treat symptoms in IBS, but in IBD, we’re fighting a war against the self. The irony? Both are rooted in a disconnection - between mind and gut, between immune system and identity. We’re not just treating bowels. We’re negotiating with the organism’s sense of self.