By January 2026, over 287 drugs remain in short supply across the U.S., with nearly half of them critical for treating heart attacks, cancer, and severe infections. Hospitals are rationing life-saving medications. Doctors are calling patients to say their prescriptions can’t be filled. And Congress? Two bills have been introduced to fix this - but they’re stuck in limbo, buried under a government shutdown that’s now lasted over 40 days.
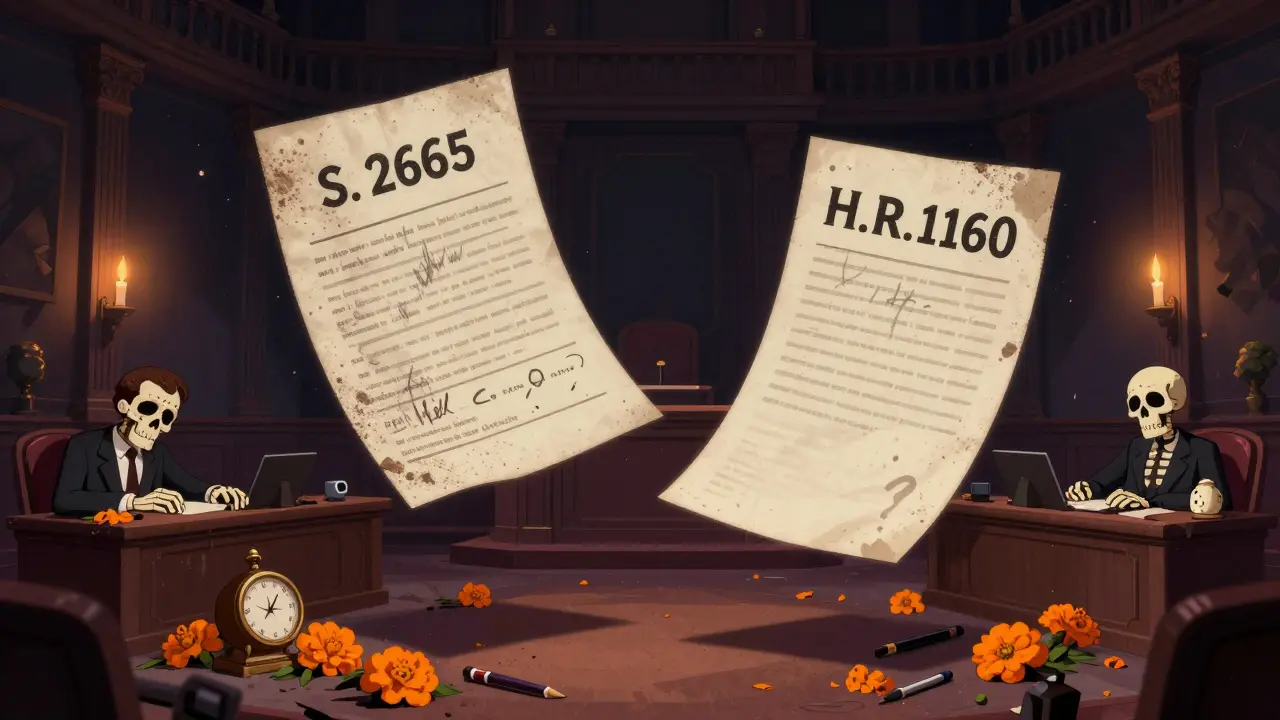
The Two Bills Trying to Fix the Crisis
The most direct response so far is the Drug Shortage Prevention Act of 2025 (S.2665). Introduced by Senator Amy Klobuchar in August 2025, this bill would force drug manufacturers to notify the FDA the moment they see a spike in demand for critical medicines. Right now, companies aren’t required to say anything until it’s too late - often after hospitals have already run out. The goal? Catch shortages before they happen. But here’s the catch: the bill doesn’t define what counts as a “critical drug,” and it doesn’t say when manufacturers must report or what happens if they don’t. No penalties. No timelines. Just a vague request.
Meanwhile, in the House, H.R.1160 - the Health Care Provider Shortage Minimization Act of 2025 - was introduced with no public summary, no sponsor list, and no committee assignment. All we know is the title. Experts believe it’s meant to tackle the growing gap between patients and doctors. Right now, 122 million Americans live in areas where there aren’t enough primary care providers. By 2034, the medical field could be short 124,000 physicians. This bill could be about funding more training programs, expanding telehealth, or relaxing licensing rules across state lines. But without the text, no one can say for sure.
Why These Bills Are Stuck
The government shut down on October 1, 2025 - the longest in U.S. history. Over 800,000 federal workers were sent home, including nearly every FDA employee who tracks drug shortages. The FDA’s Drug Shortage Portal, the main tool hospitals use to check inventory, is now outdated. Some reports haven’t been updated since September.
With no one at the FDA to review S.2665’s requirements, the bill can’t move forward. No hearings. No amendments. No votes. Even if the Senate wanted to act, they can’t. The House isn’t much better. Lawmakers are focused on cutting foreign aid and fighting over phone record lawsuits - not fixing medicine shortages.
And here’s the real problem: even if these bills passed tomorrow, they’d need money to work. The Congressional Budget Office estimates S.2665 would cost $45 million a year just to monitor and enforce. But Congress just approved $9 billion in cuts to State Department and USAID funding. That’s not going to come back for drugs.
Who’s Feeling the Pain
Hospitals are the first to notice. According to the American Hospital Association, 98% of hospitals reported at least one critical drug shortage in the third quarter of 2025. Oncologists are switching patients to less effective chemo drugs. ERs are using expired antibiotics because new ones aren’t arriving. Nurses are calling pharmacies daily, begging for a few vials of epinephrine.
Doctors aren’t just frustrated - they’re scared. A September 2025 survey by the American Medical Association found that 87% of physicians have had to change a patient’s treatment plan because a drug wasn’t available. And only 12% even knew H.R.1160 existed. That’s not awareness - that’s silence.
It’s not just hospitals. Pharmacies are running out of insulin, heart medications, and antibiotics. Generic drug makers - who produce 90% of U.S. prescriptions - say 63% of shortages come from manufacturing delays. Raw materials sit in foreign ports. Equipment breaks. And no one tells the FDA until it’s already too late.

What’s Missing From the Bills
S.2665 is a good idea, but it’s incomplete. It assumes manufacturers will report honestly and early. But what if they wait to avoid fines? What if they report too late? What if the FDA doesn’t have staff to respond? The bill doesn’t say. It’s like asking someone to call 911 - but not giving them a phone or telling them what to say.
H.R.1160 is even worse. It’s a ghost bill. No details. No sponsors. No public discussion. In a time when 1 in 3 Americans can’t get a timely doctor’s appointment, Congress is introducing a bill to fix provider shortages - and then vanishing.
Neither bill addresses the root causes: over-reliance on foreign drug ingredients, lack of domestic manufacturing capacity, or the fact that many life-saving drugs make so little profit that companies stop making them. The FDA has known this for years. But without funding or enforcement, warnings don’t turn into action.
What Comes Next
The Senate’s proposed continuing resolution would keep the government open until January 30, 2026 - but it doesn’t mention drugs or doctors once. If no deal is reached by then, the shutdown will extend, and both bills will die when the 119th Congress ends in January 2027.
That means patients will keep facing empty shelves. Hospitals will keep scrambling. And Congress will keep ignoring the crisis - until someone dies because a drug wasn’t there.
For now, the only real action is happening outside Washington. Pharmacies are pooling supplies. Telehealth clinics are shifting to alternatives. Patients are joining advocacy groups. But without legislation that’s specific, funded, and enforceable, these are just Band-Aids on a bleeding wound.
The tools to fix this exist. We know which drugs are in short supply. We know why they’re running out. We know how many doctors we need. What’s missing is the political will to act - before the next shortage kills someone who could’ve been saved.
What is the Drug Shortage Prevention Act of 2025?
The Drug Shortage Prevention Act of 2025 (S.2665) is a Senate bill introduced by Senator Amy Klobuchar that would require pharmaceutical manufacturers to notify the FDA when demand for critical drugs increases. The goal is to give regulators time to respond before shortages occur. However, the bill doesn’t define which drugs are considered “critical,” set deadlines for reporting, or outline penalties for non-compliance.
What does H.R.1160 do?
H.R.1160, the Health Care Provider Shortage Minimization Act of 2025, is a House bill with no public details. No sponsor list, no summary, no committee assignment. Experts believe it’s meant to address the nationwide shortage of doctors - especially in primary care - but without the full text, its purpose and provisions remain unknown.
Why are these bills stuck?
Both bills are stuck because of the longest government shutdown in U.S. history, which began in October 2025. The FDA, which would enforce S.2665, has been shut down. FDA staff responsible for tracking drug shortages have been furloughed. The House has not taken up H.R.1160 for review. Without functioning agencies or congressional action, these bills can’t move forward.
How many drugs are currently in short supply?
As of September 30, 2025, the FDA listed 287 drugs in short supply, with 47% classified as critical - meaning they’re used to treat life-threatening conditions like cancer, heart failure, and severe infections. The number has been rising steadily since 2022.
Are these bills likely to pass in 2026?
Unlikely. If the government shutdown continues past January 30, 2026 - the deadline in the proposed continuing resolution - both bills will expire when the 119th Congress ends in January 2027. Without funding, enforcement power, or political urgency, they won’t survive. Any real progress would require a new Congress and a renewed focus on healthcare infrastructure.


Haley Parizo
January 2, 2026 AT 16:46This isn't just policy failure-it's moral bankruptcy. We're letting people die because politicians can't stop fighting over who gets to control the levers of power. The FDA’s portal hasn’t been updated since September? That’s not bureaucracy. That’s negligence dressed in a suit. And H.R.1160? A ghost bill with no sponsor? That’s not oversight-that’s theatrical theater. They don’t want to fix this. They want to look like they care while the shelves stay empty.
Ian Ring
January 3, 2026 AT 11:34Wow. Just... wow. This is absolutely devastating. I’m from the UK, and even we don’t let things get this bad. The fact that epinephrine is being begged for? That’s not a healthcare crisis-that’s a humanitarian emergency. And the bills? They’re not broken-they’re abandoned. I’m speechless. 😔
erica yabut
January 5, 2026 AT 10:27Let’s be brutally honest: this is what happens when you let corporate lobbyists write legislation while the FDA’s staff is furloughed. S.2665 is a hollow shell wrapped in the flag of ‘action.’ It’s the legislative equivalent of handing someone a flashlight during a blackout and calling it ‘energy security.’ And H.R.1160? A silent scream in a vacuum. No sponsors? No text? That’s not incompetence-that’s contempt. You can’t legislate compassion with vagueness and silence.
Vincent Sunio
January 6, 2026 AT 01:32It is important to note that the assertion that 287 drugs are in short supply is statistically misleading without context regarding volume, duration, and geographic distribution. Furthermore, the claim that manufacturers are not required to report demand spikes is inaccurate-current FDA guidance encourages voluntary reporting under the Drug Supply Chain Security Act. The absence of penalties in S.2665 is not a flaw but a reflection of the legislative principle of incrementalism. To label this a moral failure is hyperbolic and unproductive.
Kerry Howarth
January 7, 2026 AT 18:14Even if the bills are weak, they’re the only things on the table. Let’s not pretend we’re waiting for a perfect solution. The fact that hospitals are rationing chemo drugs means we’re already past the point of ‘perfect.’ We need to take the best available tool and make it work-then fix the gaps later. Start somewhere. Anything is better than nothing.
Shruti Badhwar
January 8, 2026 AT 16:06As someone from India, I’ve seen how generic drug manufacturing collapses under supply chain fragility. The U.S. is now facing what developing nations have dealt with for decades: reliance on foreign APIs, no domestic buffer, and zero contingency planning. This isn’t a new problem-it’s a systemic failure of industrial policy. If Congress won’t act, maybe states should start mandating domestic production quotas for critical drugs. We can’t outsource survival.
Brittany Wallace
January 9, 2026 AT 09:12I keep thinking about the nurses calling pharmacies daily. That image haunts me. We talk about bills and budgets, but the real story is in those quiet, exhausted voices asking for just one vial. Maybe the answer isn’t just legislation-it’s culture. What if we treated drug access like clean water? Like fire alarms? Like air traffic control? We don’t wait for a perfect system to save lives-we build the scaffolding and keep fixing it. Let’s stop waiting for Congress to be heroes. Let’s be the ones who demand they stop being bystanders.
Michael Burgess
January 10, 2026 AT 02:35Look-I get the rage. But here’s the weird thing: the real innovation isn’t in D.C. It’s in the back rooms of rural clinics using telehealth to triage patients when insulin runs out. Pharmacies in Ohio are sharing stock across county lines. A group in Pittsburgh started a community drug bank. These aren’t flashy fixes, but they’re saving lives right now. The bills? Maybe they’ll come. But the people? They’re already doing the work. We need to amplify those stories-not just scream at the politicians.
Liam Tanner
January 11, 2026 AT 08:30It’s funny how we treat drug shortages like a surprise. We’ve been warning about this for 15 years. The same companies that made billions off opioid prescriptions now make pennies on generic antibiotics. Why would they invest in capacity? Why would they risk fines? The system was designed to fail. The bills aren’t the problem-they’re symptoms. We need to restructure the entire incentive model. Profit over people isn’t a bug. It’s the feature.
Palesa Makuru
January 11, 2026 AT 21:39Oh please. You think this is bad? Try living in a country where you pay $100 for a single vial of insulin and still can’t get it because the pharmacy’s ‘out of stock.’ At least here, you have a bill-even if it’s useless. In South Africa, we don’t even have a bill. We have silence. So yeah, complain about Congress. But don’t act like this is the worst it’s ever been. We’ve been fighting this war alone for decades. You’re just now noticing the bullets.
Hank Pannell
January 13, 2026 AT 05:22Let’s deconstruct the structural epistemology of this crisis. The pharmaceutical supply chain is a complex adaptive system with non-linear feedback loops-domestic manufacturing capacity, global raw material dependency, regulatory capture, and profit maximization algorithms all interacting. S.2665 attempts a top-down intervention without addressing the bottom-up emergent behaviors-like manufacturers delaying notifications to avoid regulatory scrutiny. H.R.1160’s opacity suggests a failure of institutional transparency. But the real issue? The political economy of healthcare in the U.S. is fundamentally misaligned with public health outcomes. The bills are not failures-they’re artifacts of a system that prioritizes capital circulation over human survival. We need systemic redesign, not incremental policy tweaks. And until we acknowledge that, we’re just rearranging deck chairs on the Titanic.