When your kidneys are damaged, high blood pressure doesn’t just make things worse-it speeds up the damage. For people with chronic kidney disease (CKD), controlling blood pressure isn’t just about avoiding heart attacks or strokes. It’s about keeping the kidneys working as long as possible. And for decades, two classes of blood pressure medications have stood out: ACE inhibitors and ARBs.
Why Blood Pressure Matters in Kidney Disease
Your kidneys filter waste and extra fluid from your blood. They also help regulate blood pressure by controlling fluid levels and releasing hormones. When kidney function drops, this system breaks down. High pressure inside the tiny filtering units-called glomeruli-forces proteins like albumin into the urine. That’s proteinuria, a key sign of kidney damage.
Left unchecked, this cycle of high pressure and protein leakage leads to scarring, loss of filtering cells, and eventually kidney failure. The goal? Lower pressure inside the kidneys, reduce protein loss, and slow decline. That’s where ACE inhibitors and ARBs come in.
How ACE Inhibitors and ARBs Work
Both drugs target the same system: the renin-angiotensin-aldosterone system (RAAS). This is your body’s natural blood pressure control network. When it’s overactive, it tightens blood vessels, holds onto salt and water, and raises pressure-especially inside the kidneys.
ACE inhibitors, like lisinopril, enalapril, and benazepril, block the enzyme that turns angiotensin I into angiotensin II. Less angiotensin II means relaxed blood vessels, less fluid retention, and lower pressure in the kidneys.
ARBs-like losartan, valsartan, and irbesartan-do something similar but differently. Instead of stopping angiotensin II from being made, they block its receptors. So even if angiotensin II is present, it can’t bind and cause damage.
The result? Both drugs reduce intraglomerular pressure, cut proteinuria by 30-50%, and slow kidney function decline by 20-40% in people with diabetes or high blood pressure. That’s not just a small benefit. It’s life-changing.
What the Evidence Shows
A landmark study in the Journal of the American Medical Association found that patients with proteinuric kidney disease who took ACE inhibitors or ARBs had a 25% lower risk of ending up on dialysis or needing a transplant compared to those on other blood pressure meds.
Even in advanced kidney disease, these drugs still help. A 2024 study tracked 1,237 patients with stage IV or V CKD-mean eGFR of just 19.8 mL/min. Those who stayed on ACE inhibitors or ARBs had a 34% lower risk of reaching kidney failure than those who stopped. No increase in death. Just slower decline.
Another UK trial followed patients with eGFR under 30 for three years. Those who kept taking their meds had better kidney function than those who stopped. No harm. Real benefit.
These aren’t outliers. Guidelines from the American College of Cardiology, American Heart Association, and KDIGO all agree: for CKD patients with proteinuria, ACE inhibitors and ARBs are first-line treatment.
ACE Inhibitors vs. ARBs: What’s the Difference?
Both work similarly to protect the kidneys. But they’re not identical.
ACE inhibitors cause a dry cough in 5-20% of users. It’s not dangerous, but it’s annoying enough that many people stop taking them. There’s also a tiny risk-0.1-0.2%-of angioedema, a swelling of the face or throat. Rare, but serious.
ARBs don’t cause cough as often. That’s why they’re often the go-to for people who can’t tolerate ACE inhibitors. They also have a lower risk of angioedema.
In terms of lowering blood pressure and reducing proteinuria, they’re about equal. So the choice often comes down to side effects, not effectiveness.

When to Use Them-and When to Be Careful
These drugs are powerful, but they’re not risk-free.
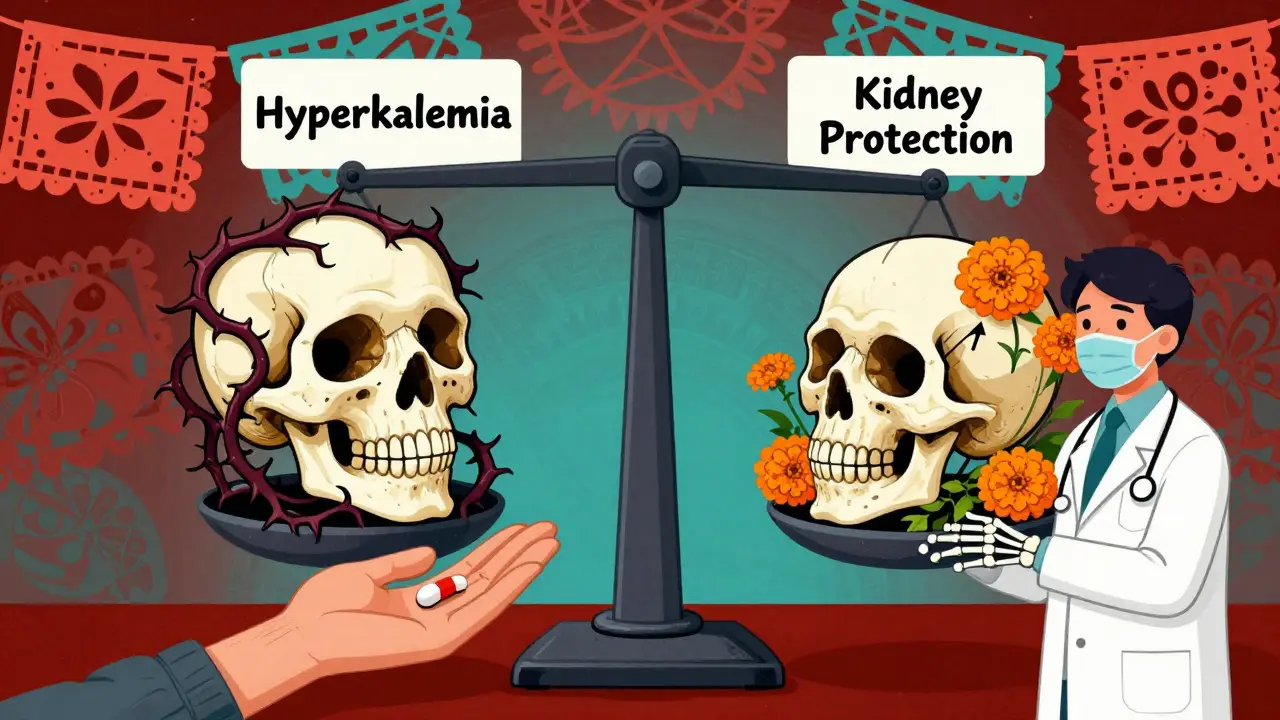
The two biggest concerns are:
- Hyperkalemia (high potassium): Happens in 10-15% of patients. Potassium builds up because RAAS blockers reduce aldosterone, which normally helps kidneys flush out potassium.
- Acute kidney injury: A temporary drop in eGFR of more than 30% can happen in 5-10% of people after starting the drug. This isn’t always bad-it can mean the drug is working by reducing pressure in the kidneys. But it needs monitoring.
That’s why doctors check kidney function and potassium before starting, then again in 1-2 weeks. If eGFR drops more than 30% or potassium goes above 5.5 mmol/L, the dose is lowered or stopped.
Here’s the myth: Don’t use these drugs in advanced CKD. That’s outdated. The 2023 KDIGO guidelines say: keep using them if eGFR is above 15 mL/min and potassium is below 5.0 mmol/L. Stopping them in late-stage CKD doesn’t protect the kidneys-it harms them.
Dual Therapy: ACE + ARB Together?
Some studies show combining an ACE inhibitor with an ARB reduces proteinuria even more-by up to 35%. Sounds great, right?
But here’s the catch: the Veterans Affairs Nephropathy Trial found dual therapy doubled the risk of acute kidney injury and increased hyperkalemia by 50%. No improvement in long-term kidney outcomes. No survival benefit.
So current guidelines strongly advise against combining them. One or the other, at the highest tolerated dose, is the standard.
Who Should Be Taking These Drugs?
Not everyone with kidney disease needs them. But if you have:
- Chronic kidney disease (any stage) with proteinuria (albumin-to-creatinine ratio >30 mg/g)
- Diabetes and kidney damage
- High blood pressure and CKD
…then you’re a candidate. Even if your blood pressure is normal. These drugs protect the kidneys beyond just lowering pressure.
And yes-even if your eGFR is low. A 2024 study showed patients with eGFR below 20 still gained protection. The key is monitoring, not avoidance.
Real Patient Experiences
On patient forums, stories vary. One person on Reddit with stage 4 CKD has been on lisinopril for five years. Quarterly blood tests. Stable eGFR. No side effects.
Another stopped their ARB after a sudden eGFR drop. Turned out they’d been dehydrated. Restarted the drug after rehydration-and their kidney numbers improved.
But 28% of people quit ACE inhibitors because of the cough. 12% stopped due to high potassium, which meant cutting back on bananas, potatoes, and salt substitutes.
It’s not perfect. But for most, the trade-off is worth it.
Monitoring: The Key to Safe Use
These drugs aren’t set-and-forget. They need attention.
Here’s what works:
- Test eGFR and serum potassium before starting.
- Check again 1-2 weeks after starting or changing dose.
- Keep checking every 1-3 months once stable.
- Stop or reduce dose if eGFR drops >30% or potassium >5.5 mmol/L.
- Never stop abruptly-talk to your doctor.
And if you’re on a diuretic or NSAIDs (like ibuprofen), tell your doctor. Those can raise potassium and make kidney drops worse.
What’s Next? New Drugs on the Horizon
Researchers are looking at next-gen RAAS blockers. One, sacubitril/valsartan (Entresto), was originally for heart failure but now shows promise for kidneys too. In a 2024 trial extension, it slowed kidney decline by 22% compared to enalapril in patients with both heart failure and CKD.
It’s not approved for kidney disease yet-but it’s a sign that the field is evolving. For now, ACE inhibitors and ARBs remain the gold standard.
The Bottom Line
High blood pressure and kidney disease are a dangerous pair. ACE inhibitors and ARBs break that cycle. They’re not magic, but they’re among the most proven tools we have.
Underuse is still a problem. Only about 58% of patients with advanced CKD get them, even though guidelines say they should. Fear of side effects has kept too many people from getting the benefit.
With proper monitoring, these drugs are safe-even in late-stage kidney disease. The risks of stopping them are greater than the risks of taking them.
If you have kidney disease and high blood pressure-or even just protein in your urine-ask your doctor: Should I be on an ACE inhibitor or ARB? Don’t assume you’re too far along. You might still have time to protect your kidneys.
Are ACE inhibitors and ARBs safe for people with advanced kidney disease?
Yes, when monitored properly. Studies show that continuing ACE inhibitors or ARBs in stage IV or V CKD slows kidney failure progression by 34% compared to stopping them. The key is regular blood tests for potassium and eGFR. If potassium stays under 5.0 mmol/L and eGFR doesn’t drop more than 30%, these drugs are safe and beneficial-even when kidney function is low.
Why do some people stop taking ACE inhibitors?
The most common reason is a persistent dry cough, which affects 5-20% of users. It’s not dangerous, but it’s irritating enough that many stop. A small number also experience angioedema-a rare but serious swelling of the face or throat. For these patients, switching to an ARB usually solves the problem without losing kidney protection.
Can I take an ACE inhibitor and ARB together for better results?
No. While combining them reduces proteinuria slightly more, it also doubles the risk of acute kidney injury and increases hyperkalemia by 50%. Major guidelines, including KDIGO and the American Heart Association, strongly advise against dual therapy. One drug at the highest tolerated dose is safer and just as effective for long-term kidney protection.
How long does it take for ACE inhibitors or ARBs to protect the kidneys?
The blood pressure-lowering effect happens within days. But kidney protection-reducing proteinuria and slowing decline-takes weeks to months. Most patients see reduced protein in their urine within 4-8 weeks. The full benefit on kidney function may take 6-12 months to become clear. Consistency matters more than speed.
Do I need to change my diet if I’m on an ACE inhibitor or ARB?
Yes, especially if your potassium is rising. Avoid high-potassium foods like bananas, oranges, potatoes, tomatoes, and salt substitutes containing potassium chloride. Limit processed foods, which often have hidden potassium. Your doctor or dietitian can help you adjust your diet based on your blood test results. Don’t stop the medication-adjust your diet instead.
What if my blood pressure is already normal? Do I still need these drugs?
Yes. ACE inhibitors and ARBs protect the kidneys independently of blood pressure. Even if your BP is normal, if you have protein in your urine or diabetes with kidney disease, these drugs reduce protein leakage and slow scarring. They’re not just blood pressure pills-they’re kidney protectors.
Can I stop taking these drugs if my kidney function improves?
Don’t stop without talking to your doctor. Even if your eGFR improves or proteinuria decreases, stopping the medication can cause a rebound in kidney damage. These drugs work by changing the internal environment of the kidney. Stopping them removes that protection. Long-term use is usually needed for ongoing benefit.


Prasanthi Kontemukkala
December 25, 2025 AT 16:15Just wanted to say thank you for this clear breakdown. I’m a nurse in Kerala and see so many patients stop these meds because they’re scared of side effects. This helps me explain why staying on them matters-even when eGFR is low. You’re right, the fear is worse than the risk.
Alex Ragen
December 25, 2025 AT 18:30One must interrogate the epistemological foundations of RAAS inhibition: is it truly the drug, or the *ontological shift* in renal hemodynamics that confers protection? The reduction in proteinuria is merely a phenomenological marker-what we’re really observing is the dissolution of pathological intraglomerular tension…
…and yet, the data remains stubbornly empirical. Fascinating, isn’t it? How the body obeys mathematical laws even when we fail to comprehend them.
Lori Anne Franklin
December 26, 2025 AT 16:36My dad’s been on losartan for 7 years with stage 3 CKD-his proteinuria dropped from 800 to 200 mg/g and his eGFR hasn’t budged. He eats bananas like it’s his job 😄. If you’re monitoring, this stuff works. Don’t let a dry cough scare you off!
Dan Alatepe
December 28, 2025 AT 02:39Bro… I was on lisinopril and that cough? 😭 Like my throat was holding a silent scream every night. Switched to valsartan and it was like my lungs got a VIP pass to chill mode. Also, potassium? I swapped my sweet potato fries for zucchini noodles. No drama. Just peace.
Matthew Ingersoll
December 28, 2025 AT 23:16Interesting how this mirrors the evolution of hypertension treatment in sub-Saharan Africa. We used to avoid these drugs in advanced CKD out of fear. Now, with better lab access, we’re seeing survival benefits even at eGFR <20. The data doesn’t lie-it’s just not always available.
carissa projo
December 30, 2025 AT 00:14I love how this article doesn’t just list facts-it tells a story. The kidneys aren’t broken machines needing repair; they’re delicate ecosystems. ACEi and ARBs don’t fix them-they gently quiet the storm inside. That’s poetry disguised as pharmacology.
And to those who quit because of potassium… maybe your body’s just asking you to eat less processed food, not stop your medicine. Listen. Adjust. Stay.
josue robert figueroa salazar
December 30, 2025 AT 06:54Stop taking them = bad. Keep taking = good. Monitoring = key. Dual therapy = dumb. Cough = annoying. Potassium = watch it. Done.
david jackson
December 30, 2025 AT 17:25I’ve been reading everything I can on this because my mom has stage 4 CKD and was told to stop her ARB last year. She’s now on dialysis. I found that 2024 study you mentioned-the one with 1,237 patients-and I cried. Not because it was sad, but because it felt like a secret they didn’t want us to know. Why aren’t we pushing this harder? Why are we still letting people fall through the cracks because someone thought ‘low eGFR = avoid RAAS blockers’? It’s not just medical ignorance-it’s systemic neglect.
Jody Kennedy
December 30, 2025 AT 22:54Just got my first ACEi prescription after years of ‘normal BP so I don’t need it’ nonsense. Turns out my ACR was 450. My doctor said, ‘This isn’t about your blood pressure-it’s about your kidneys.’ I’m scared but also… hopeful. I’m gonna track my potassium like it’s my job. Thanks for the clarity!
christian ebongue
December 31, 2025 AT 20:04so u mean i cant have my potassium chloride salt anymore? 😬 guess i’m gonna have to taste my food now… not just the sodium.
Joanne Smith
January 2, 2026 AT 19:09That 28% who quit because of the cough? I was one of them. Switched to ARB. No cough. Still protecting my kidneys. But here’s the thing-no one told me the cough could be delayed. I started lisinopril, felt fine for 3 months… then BAM. Cough like a chain-smoker with a cold. If I’d known, I’d have switched sooner. Don’t wait. Talk to your doc before you quit.
Bryan Woods
January 4, 2026 AT 03:11Thank you for compiling this with such precision. The evidence is overwhelming. The challenge lies in translation-ensuring patients understand that kidney protection isn’t contingent on BP numbers. This is not a hypertension protocol-it’s a nephroprotective strategy. I will be sharing this with my clinic.